Professor Hardev Pandha
About
Biography
Hardev Pandha is a clinician scientist and medical oncologist who graduated in medicine at the University of Birmingham. He trained in internal medicine and subsequently in medical oncology at the Royal Postgraduate Medical School at Hammersmith Hospital, London. He completed his PhD (Imperial College) in the Imperial Cancer Research Fund labs at the Hammersmith. He was a visiting fellow at Stanford University prior to completing his medical oncology training at the Royal Marsden Hospital, London. He was a senior lecturer in tumour immunology and medical oncology at St Georges, University of London in 2000 before being appointed Prof of Urological Oncology at the University of Surrey in 2006.
His areas of expertise include the management of patients with Urological cancers and malignant melanoma. He has a key interest in early phase clinical trials involving targeted agents and the translational aspects of novel therapies. His portfolio includes gene and viral therapy as well as immunotherapy and small molecule inhibitors. His laboratory interests reflect this and in particular a combination of novel and biological therapies with more conventional treatments. His lab team have evolved a robust infrastructure of patient sample procurement and biobanking for translational research.
News
In the media
ResearchResearch interests
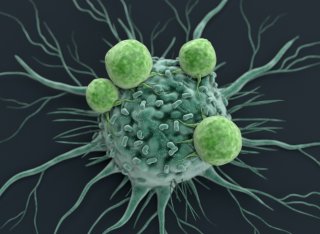
- Tumour immunology
- Urological cancer
- Gene therapy
Research interests
- Tumour immunology
- Urological cancer
- Gene therapy
Publications
Highlights
- The Role of Circular RNAs in Pancreatic Ductal Adenocarcinoma and Biliary-Tract Cancers. Limb C, Liu DSK, Veno MT, Rees E, Krell J, Bagwan IN, Giovannetti E, Pandha H, Strobel O, Rockall TA, Frampton AE.Limb C, et al. Cancers (Basel). 2020 Nov 4;12(11):E3250.
- An integrative multi-omics analysis to identify candidate DNA methylation biomarkers related to prostate cancer risk. Wu L, Yang Y, Guo X, Shu XO, Cai Q, Shu X, Li B, Tao R, Wu C, Nikas JB, Sun Y, Zhu J, Roobol MJ, Giles GG, Brenner H, John EM, Clements J, Grindedal EM, Park JY, Stanford JL, Kote-Jarai Z, Haiman CA, Eeles RA, Zheng W, Long J; PRACTICAL consortium; CRUK Consortium; BPC3 Consortium; CAPS Consortium; PEGASUS Consortium.Wu L, et al. Nat Commun. 2020 Aug 6;11(1):3905.
- A Genetic Risk Score to Personalize Prostate Cancer Screening, Applied to Population Data. Huynh-Le MP, Fan CC, Karunamuni R, Walsh EI, Turner EL, Lane JA, Martin RM, Neal DE, Donovan JL, Hamdy FC, Parsons JK, Eeles RA, Easton DF, Kote-Jarai Z, Amin Al Olama A, Benlloch Garcia S, Muir K, Grönberg H, Wiklund F, Aly M, Schleutker J, Sipeky C, Tammela TL, Nordestgaard BG, Key TJ, Travis RC, Pharoah PDP, Pashayan N, Khaw KT, Thibodeau SN, McDonnell SK, Schaid DJ, Maier C, Vogel W, Luedeke M, Herkommer K, Kibel AS, Cybulski C, Wokolorczyk D, Kluzniak W, Cannon-Albright LA, Brenner H, Schöttker B, Holleczek B, Park JY, Sellers TA, Lin HY, Slavov CK, Kaneva RP, Mitev VI, Batra J, Clements JA, Spurdle AB, Teixeira MR, Paulo P, Maia S, Pandha H, Michael A, Mills IG, Andreassen OA, Dale AM, Seibert TM; Australian Prostate Cancer BioResource (APCB); PRACTICAL Consortium.Huynh-Le MP, et al. Cancer Epidemiol Biomarkers Prev. 2020 Sep;29(9):1731-1738.
- The effect of sample size on polygenic hazard models for prostate cancer. Karunamuni RA, Huynh-Le MP, Fan CC, Eeles RA, Easton DF, Kote-Jarai Z, Amin Al Olama A, Benlloch Garcia S, Muir K, Gronberg H, Wiklund F, Aly M, Schleutker J, Sipeky C, Tammela TLJ, Nordestgaard BG, Key TJ, Travis RC, Neal DE, Donovan JL, Hamdy FC, Pharoah P, Pashayan N, Khaw KT, Thibodeau SN, McDonnell SK, Schaid DJ, Maier C, Vogel W, Luedeke M, Herkommer K, Kibel AS, Cybulski C, Wokolorczyk D, Kluzniak W, Cannon-Albright L, Brenner H, Schöttker B, Holleczek B, Park JY, Sellers TA, Lin HY, Slavov C, Kaneva R, Mitev V, Batra J, Clements JA, Spurdle A; Australian Prostate Cancer BioResource (APCB), Teixeira MR, Paulo P, Maia S, Pandha H, Michael A, Mills IG, Andreassen OA, Dale AM, Seibert TM; PRACTICAL Consortium.Karunamuni RA, et al. Eur J Hum Genet. 2020 Oct;28(10):1467-1475.
- Genomic analysis of male puberty timing highlights shared genetic basis with hair colour and lifespan. Hollis B, Day FR, Busch AS, Thompson DJ, Soares ALG, Timmers PRHJ, Kwong A, Easton DF, Joshi PK, Timpson NJ; PRACTICAL Consortium; 23andMe Research Team, Ong KK, Perry JRB.Hollis B, et al.Nat Commun. 2020 Mar 24;11(1):1536.
- Modifying the Non-muscle Invasive Bladder Cancer Immune Microenvironment for Optimal Therapeutic Response. Annels NE, Simpson GR, Pandha H.Annels NE, et al. Front Oncol. 2020 Feb 18;10:175
- The PERK Inhibitor GSK2606414 Enhances Reovirus Infection in Head and Neck Squamous Cell Carcinoma via an ATF4-Dependent Mechanism. McLaughlin M, Pedersen M, Roulstone V, Bergerhoff KF, Smith HG, Whittock H, Kyula JN, Dillon MT, Pandha HS, Vile R, Melcher AA, Harrington KJ.McLaughlin M, et al. Mol Ther Oncolytics. 2020 Jan 17;16:238-249.
- Rationale and design of the POLEM trial: avelumab plus fluoropyrimidine-based chemotherapy as adjuvant treatment for stage III mismatch repair deficient or POLE exonuclease domain mutant colon cancer: a phase III randomised study. Lau D, Kalaitzaki E, Church DN, Pandha H, Tomlinson I, Annels N, Gerlinger M, Sclafani F, Smith G, Begum R, Crux R, Gillbanks A, Wordsworth S, Chau I, Starling N, Cunningham D, Dhillon T.Lau D, et al. ESMO Open. 2020 Feb;5(1):e000638.
- PBX3 in Cancer. Morgan R, Pandha HS.Morgan R, et al. Cancers (Basel). 2020 Feb 13;12(2):431.
- APOBEC3B-mediated corruption of the tumor cell immunopeptidome induces heteroclitic neoepitopes for cancer immunotherapy. Driscoll CB, Schuelke MR, Kottke T, Thompson JM, Wongthida P, Tonne JM, Huff AL, Miller A, Shim KG, Molan A, Wetmore C, Selby P, Samson A, Harrington K, Pandha H, Melcher A, Pulido JS, Harris R, Evgin L, Vile RG.Driscoll CB, et al.. Nat Commun. 2020 Feb 7;11(1):790.
- A Specific Blood Signature Reveals Higher Levels of S100A12: A Potential Bladder Cancer Diagnostic Biomarker Along With Urinary Engrailed-2 Protein Detection. Elamin AA, Klunkelfuß S, Kämpfer S, Oehlmann W, Stehr M, Smith C, Simpson GR, Morgan R, Pandha H, Singh M. Front Oncol. 2020 Jan 9;9:1484.
- The Open University's first one-day symposium on treatment-emergent neuroendocrine prostate cancer. Mather RL, Andrews H, Pandha H, Jachetti E, Micallef J, Wang Y, Crea F. Future Oncol. 2020 Feb;16(6):147-149.
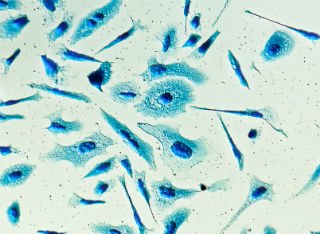
Oncolytic viruses are biological agents which can easily be delivered at high doses directly to the bladder through a catheter (intravesical), with low risk of systemic uptake and toxicity. To date, a number of viruses have been delivered intravesically in patients and in murine models with bladder cancer and antitumour effects demonstrated. Here, we describe in vitro methods to evaluate Coxsackie virus, CVA21, as an oncolytic virus for the treatment of human bladder cancer by determining the susceptibility of bladder cancer cell lines expressing differing levels of ICAM-1 surface receptor to CVA21.
Simple Summary Pancreatic and biliary tract cancers often present with non-specific symptoms, resulting in diagnosis at a late stage. This may be too late for curative surgery. Earlier detection and characterisation may guide treatment options and increase survival. Natural "circles" of RNA (circRNAs) are shown to regulate cancer-related genes, and act as cancer "biomarkers". Recent research has shown that circRNAs are both abundant and stable, both of which are desirable characteristics for clinically useful biomarkers. In this systematic review, we describe the roles of circRNAs in pancreatic and biliary tract cancers, summarise the current published research and explore their utility as a biomarker. A total of 32 articles were included: 22 considering Pancreatic Cancer, 7 for Bile Duct Cancer and 3 for Gallbladder Cancer. CircRNA proved an exciting prospect as a biomarker for these cancers and future work should continue to develop and expand this field of research. Pancreatic Ductal Adenocarcinoma (PDAC) and biliary-tract cancers (BTC) often present at a late stage, and consequently patients have poor survival-outcomes. Circular RNAs (circRNAs) are non-coding RNA molecules whose role in tumourigenesis has recently been realised. They are stable, conserved and abundant, with tissue-specific expression profiles. Therefore, significant interest has arisen in their use as potential biomarkers for PDAC and BTC. High-throughput methods and more advanced bioinformatic techniques have enabled better profiling and progressed our understanding of how circRNAs may function in the competing endogenous RNA (ceRNA) network to influence the transcriptome in these cancers. Therefore, the aim of this systematic review was to describe the roles of circRNAs in PDAC and BTC, their potential as biomarkers, and their function in the wider ceRNA network in regulating microRNAs and the transcriptome. Medline, Embase, Scopus and PubMed were systematically reviewed to identify all the studies addressing circRNAs in PDAC and BTC. A total of 32 articles were included: 22 considering PDAC, 7 for Cholangiocarcinoma (CCA) and 3 for Gallbladder Cancer (GBC). There were no studies investigating Ampullary Cancer. Dysregulated circRNA expression was associated with features of malignancy in vitro, in vivo, and ex vivo. Overall, there have been very few PDAC and BTC tissues profiled for circRNA signatures. Therefore, whilst the current studies have demonstrated some of their functions in these cancers, further work is required to elucidate their potential role as cancer biomarkers in tissue, biofluids and biopsies.
Reovirus type 3 Dearing (reovirus) is a tumor-selective oncolytic virus currently under evaluation in clinical trials. Here, we report that the therapeutic efficacy of reovirus in head and neck squamous cell cancer can be enhanced by targeting the unfolded protein response (UPR) kinase, protein kinase R (PKR)-like endoplasmic reticulum kinase (PERK). PERK inhibition by GSK2606414 increased reovirus efficacy in both 2D and 3D models in vitro, while perturbing the normal host cell response to reovirus-induced endoplasmic reticulum (ER) stress. UPR reporter constructs were used for live-cell 3D spheroid imaging. Profiling of eIF2a-ATF4, IRE1a-XBP1, and ATF6 pathway activity revealed a context-dependent increase in eIF2a-ATF4 signaling due to GSK2606414. GSK2606414 blocked eIF2a-ATF4 signaling because of the canonical ER stress agent thapsigargin. In the context of reovirus infection, GSK2606414 induced eIF2a-ATF4 signaling. Knockdown of eIF2a kinases PERK, GCN2, and PKR revealed eIF2a-ATF4 reporter activity was dependent on either PERK or GCN2. Knockdown of ATF4 abrogated the GSK2606414-induced increase in reovirus protein levels, confirming eIF2a-ATF signaling as key to the observed phenotype. Our work identifies a novel approach to enhance the efficacy and replication of reovirus in a therapeutic setting.
Prostate cancer is a highly heritable disease with large disparities in incidence rates across ancestry populations. We conducted a multiancestry meta-analysis of prostate cancer genome-wide association studies (107,247 cases and 127,006 controls) and identified 86 new genetic risk variants independently associated with prostate cancer risk, bringing the total to 269 known risk variants. The top genetic risk score (GRS) decile was associated with odds ratios that ranged from 5.06 (95% confidence interval (CI), 4.84-5.29) for men of European ancestry to 3.74 (95% CI, 3.36-4.17) for men of African ancestry. Men of African ancestry were estimated to have a mean GRS that was 2.18-times higher (95% CI, 2.14-2.22), and men of East Asian ancestry 0.73-times lower (95% CI, 0.71-0.76), than men of European ancestry. These findings support the role of germline variation contributing to population differences in prostate cancer risk, with the GRS offering an approach for personalized risk prediction.
Purpose: The CANON (CAVATAK in NON-muscle invasive bladder cancer) study evaluated a novel ICAM-1-targeted immunotherapeutic-coxsackievirus A21 as a novel oncolytic agent against bladder cancer. Experimental Design: Fifteen patients enrolled on this 'window of opportunity' phase 1 study, exposing primary bladder cancers to CAVATAK prior to surgery. The first nine patients received intravesical administration of monotherapy CAVATAK; in the second stage, six patients received CAVATAK with a sub-therapeutic dose of mitomycinC, known to enhance expression of ICAM-1 on bladder cancer cells. The primary endpoint was to determine patient safety and maximum tolerated dose. Secondary endpoints were evidence of viral replication, induction of inflammatory cytokines, anti-tumour activity and viral-induced changes in resected tissue. Results: Clinical activity of CAVATAK was demonstrated by induction of tumour inflammation and haemorrhage following either single or multiple administrations of CAVATAK in multiple patients, and a complete resolution of tumour in one patient. Whether used alone or in combination with mitomycinC, CAVATAK caused marked inflammatory changes within NMIBC tissue biopsies by up-regulating interferon-inducible genes including both immune checkpoint-inhibitory genes (PD-L1 and LAG3) and Th1-associated chemokines as well as induction of the innate activator RIG-I, compared to bladder cancer tissue from untreated patients. No significant toxicities were reported in any patient, from either virus or combination therapy. Conclusions: The acceptable safety profile of CAVATAK, proof of viral targeting, replication and tumour cell death together with the virus-mediated increases in "immunological heat" within the tumour microenvironment all indicate that CAVATAK may be potentially considered as a novel therapeutic for NMIBC.
Oncolytic viruses (OVs) encoding a variety of transgenes have been evaluated as therapeutic tools to increase the efficacy of chimeric antigen receptor (CAR)-modified T cells in the solid tumor microenvironment (TME). Here, using systemically delivered OVs and CAR T cells in immunocompetent mouse models, we have defined a mechanism by which OVs can potentiate CAR T cell efficacy against solid tumor models of melanoma and glioma. We show that stimulation of the native T cell receptor (TCR) with viral or virally encoded epitopes gives rise to enhanced proliferation, CAR-directed antitumor function, and distinct memory phenotypes. In vivo expansion of dual-specific (DS) CAR T cells was leveraged by in vitro preloading with oncolytic vesicular stomatitis virus (VSV) or reovirus, allowing for a further in vivo expansion and reactivation of T cells by homologous boosting. This treatment led to prolonged survival of mice with subcutaneous melanoma and intracranial glioma tumors. Human CD19 CAR T cells could also be expanded in vitro with TCR reactivity against viral or virally encoded antigens and was associated with greater CAR-directed cytokine production. Our data highlight the utility of combining OV and CAR T cell therapy and show that stimulation of the native TCR can be exploited to enhance CAR T cell activity and efficacy in mice.
Objective To assess the efficacy and tolerability of rechallenge with sunitinib and other targeted therapies (TTs) in patitents with relapsed recurrent renal cell carcinoma (RCC) in the advanced setting. Methods In this multi-institutional retrospective study, patients with relapsed RCC were rechallenged with sunitinib or other systemic TTs as a first-line therapeutic approach after failed adjuvant sunitinib treatment. Patient characteristics, treatments and clinical outcomes were recorded. The primary endpoint was progression-free survival (PFS). Secondary endpoints were objective response rate (ORR) and overall survival (OS). Results A total of 34 patients with relapses were recorded, and 25 of these (73.5%) were men. Twenty-five patients were treated with systemic TT: 65% of patients received TT against the vascular endothelial growth factor pathway (including sunitinib), 21.7% received mammalian target of rapamycin inhibitors and 13% received immunotherapy. The median (interquartile range) time to relapse was 20.3 (5.2-20.4) months from diagnosis, and 7.5 months (1.0-8.5) from the end of adjuvant suntinib treatment. At a median follow-up of 23.5 months, 24 of the 25 patients had progressed on first-line systemic therapy. The median PFS was 12.0 months (95% confidence interval [CI] 5.78-18.2). There were no statistical differences in PFS between different treatments or sunitinib rechallenge. PFS was not statistically different in patients relapsing on or after adjuvant suntinib treatment (6 months after adjuvant suntinib ending). The ORR was 20.5%. The median OS was 29.1 months (95% CI 16.4-41.8). Conclusions Rechallenge with sunitinib or other systemic therapies is still a feasible therapeutic option that provides patients with advanced or metastastic RCC with additional clinical benefits with regard to PFS and OS after failed response to adjuvant sunitinib.
Risk classification for prostate cancer (PCa) aggressiveness and underlying mechanisms remain inadequate. Interactions between single nucleotide polymorphisms (SNPs) may provide a solution to fill these gaps. To identify SNP-SNP interactions in the four pathways (the angiogenesis-, mitochondria-, miRNA-, and androgen metabolism-related pathways) associated with PCa aggressiveness, we tested 8587 SNPs for 20,729 cases from the PCa consortium. We identified 3 KLK3 SNPs, and 1083 (P
This fully updated volume explores recently improved avenues to study urothelial carcinomas. Beginning with several novel chapters on molecular characterization and urothelial carcinogenesis, the book continues with sections on cellular and animal models, biomarkers, and approaches for targeted therapy. Written for the highly successful Methods in Molecular Biology series, chapters include introductions to their respective topics, lists of the necessary materials and reagents, step-by-step and readily reproducible laboratory protocols, as well as tips on troubleshooting and avoiding known pitfalls. Authoritative and practical, Urothelial Carcinoma: Methods and Protocols, Second Edition serves as a valuable resource to further increase our knowledge on urothelial carcinoma and also to aid research on numerous other cancers.
© 2013 Springer-Verlag London. All rights are reserved.The approval in April 2010 by the FDA in the USA of a prostate cancer vaccine (Sipuleucel-T, Provenge, Dendreon Inc.) may herald a new era in T-cell-directed cancer therapies. The magnitude of scientific effort to reach this point should not be underestimated. The key has been unraveling the complex mechanisms between the recognition of tumor antigen, breaking immune tolerance, and generation of a long-lasting and clinically meaningful cellular response. Therapeutic vaccines (i.e., vaccines for patients with ongoing disease) have two objectives: priming Ag-specific T cells and reprogramming memory T cells (i.e., a transformation from one type of immunity to another, for example, regulatory to cytotoxic). Numerous therapeutic approaches have been tested in prostate cancer patients, including autologous and allogeneic tumor cells modified to express various cytokines, peptides, proteins, and DNA vaccines. The evolution of cellular vaccines includes addressing the local immunosuppressive tumor microenvironment, modulating immune response through checkpoint blockade and, importantly, combining cellular immunotherapy with other treatment modalities such as chemotherapy exploiting their intrinsic immunomodulatory properties.
Circulating insulin-like growth factors (IGFs) and their binding proteins (IGFBPs) are associated with prostate cancer. Using genetic variants as instruments for IGF peptides, we investigated whether these associations are likely to be causal. We identified from the literature 56 single nucleotide polymorphisms (SNPs) in the IGF axis previously associated with biomarker levels (8 from a genome-wide association study [GWAS] and 48 in reported candidate genes). In ∼700 men without prostate cancer and two replication cohorts (N ∼ 900 and ∼9,000), we examined the properties of these SNPS as instrumental variables (IVs) for IGF-I, IGF-II, IGFBP-2 and IGFBP-3. Those confirmed as strong IVs were tested for association with prostate cancer risk, low (< 7) vs. high (≥ 7) Gleason grade, localised vs. advanced stage, and mortality, in 22,936 controls and 22,992 cases. IV analysis was used in an attempt to estimate the causal effect of circulating IGF peptides on prostate cancer. Published SNPs in the IGFBP1/IGFBP3 gene region, particularly rs11977526, were strong instruments for IGF-II and IGFBP-3, less so for IGF-I. Rs11977526 was associated with high (vs. low) Gleason grade (OR per IGF-II/IGFBP-3 level-raising allele 1.05; 95% CI: 1.00, 1.10). Using rs11977526 as an IV we estimated the causal effect of a one SD increase in IGF-II (∼265 ng/mL) on risk of high vs. low grade disease as 1.14 (95% CI: 1.00, 1.31). Because of the potential for pleiotropy of the genetic instruments, these findings can only causally implicate the IGF pathway in general, not any one specific biomarker.
Oncolytic viruses are multifunctional anticancer agents with huge clinical potential, and have recently passed the randomized Phase III clinical trial hurdle. Both wild-type and engineered viruses have been selected for targeting of specific cancers, to elicit cytotoxicity, and also to generate antitumor immunity. Single-agent oncolytic virotherapy treatments have resulted in modest effects in the clinic. There is increasing interest in their combination with cytotoxic agents, radiotherapy and immune-checkpoint inhibitors. Similarly to oncolytic viruses, the benefits of chemotherapeutic agents may be that they induce systemic antitumor immunity through the induction of immunogenic cell death of cancer cells. Combining these two treatment modalities has to date resulted in significant potential in vitro and in vivo synergies through various mechanisms without any apparent additional toxicities. Chemotherapy has been and will continue to be integral to the management of advanced cancers. This review therefore focuses on the potential for a number of common cytotoxic agents to be combined with clinically relevant oncolytic viruses. In many cases, this combined approach has already advanced to the clinical trial arena.
Oncolytic viruses are anticancer agents that selectively target and kill cancer cells by direct lysis, while at the same time stimulating a tumor antigen-specific adaptive immune response. These promising therapeutic agents target multiple cancers and have already proven to be an effective treatment option for solid malignancies. One such agent, T-Vec (Talimogene laherparepvec) has been licensed and is in routine clinical use for treatment of malignant melanoma.Non-muscle invasive bladder cancer (NMIBC) is an ideal potential target for oncolytic immunotherapy as locally instilled live biological therapy using Bacille Calmette-Guerin (BCG) is already well established in the clinical setting. Coxsackievirus A21 (CVA21) is a novel intercellular adhesion molecule-1 (ICAM-1)-targeted immunotherapeutic virus. We have investigated CVA21-induced cytotoxicity in a panel of human bladder cancer cell lines, revealing a range of sensitivities largely correlating with expression of the viral receptor ICAM-1. CVA21 in combination with low doses of mitomycin-C enhanced CVA21 viral replication and oncolysis by increasing surface expression levels of ICAM-1. In addition to cell lines and an animal model a key component of our studies into oncolytic immunotherapy for bladder cancer was the use of a bladder tumor precision slice preclinical model system which represents tumor architecture, heterogeneity, and the complexity of a tumor in vitro. Results seen in cell lines were reflected in the tumor slice model whereby levels of virus protein expression and induction of apoptosis were enhanced with prior exposure to mitomycin-C. In this chapter we demonstrate the utility of the precision cut tumor slice model as a unique organotypic model to test oncolytic viruses. We will describe how to prepare and slice the tumor using a vibrating microtome together with the optimum culture and conditions for treatment.
Basal cell carcinoma of the prostate (BCP) is a neoplasm composed of prostatic basal cells. There are only a few publications outlining the diagnosis, treatment, prognosis and outcome for BCP. Traditionally surgery has been used but these tumors also respond to concomitant chemo-radiotherapy. Using a BCP case report treated with radical chemo-radiotherapy from a chemotherapy regimen used in anal cancers, we propose an alternative management to the traditional options of radical surgery and radical radiotherapy.
Oncolytic reovirus is currently under active investigation in a range of tumour types. Early phase studies have shown that this agent has modest monotherapy efficacy and its future development is likely to focus on combination regimens with cytotoxic chemotherapy. Indeed, phase I/II clinical trials have confirmed that reovirus can be safely combined with cytotoxic drugs, including a platin-taxane doublet regimen, which is currently being tested in a phase III clinical trial in patients with relapsed/metastatic head and neck cancer. Therefore, we have tested this triple (reovirus, cisplatin, paclitaxel) combination therapy in a panel of four head and neck cancer cell lines. Using the combination index (CI) method, the triple therapy demonstrated synergistic cytotoxicity in vitro in both malignant and non-malignant cell lines. In head and neck cancer cell lines, this was associated with enhanced caspase 3 and 7 cleavage, but no increase in viral replication. In vitro analyses confirmed colocalisation of markers of reovirus infection and caspase 3. Triple therapy was significantly more effective than reovirus or cisplatin-paclitaxel in athymic nude mice. These data suggest that the combination of reovirus plus platin-taxane doublet chemotherapy has significant activity in head and neck cancer and underpin the current phase III study in this indication.Gene Therapy advance online publication, 16 August 2012; doi:10.1038/gt.2012.68.
Transduction of 11 pancreatic cancer cell lines with a replication-deficient adenovirus 5 expressing enhanced green fluorescent protein (Ad5EGFP) was analyzed and variable EGFP levels were observed, ranging from
Anti-angiogenic agents targeting tumour vasculature have an established place in clinical practice, and new data are constantly emerging. However, despite rapid clinical uptake, a very large number of questions regarding these agents remain unanswered. One of the main hurdles in clinical practice is lack of accurate and feasible ways of assessing response to drug beyond tumour reduction on conventional imaging. This review summarises recent developments in the field of biomarkers of response to anti-VEGF drugs.
There are currently numerous oncolytic viruses undergoing clinical trial evaluation in cancer patients and one agent,Talimogene laherparepvec, has been approved for the treatment of malignant melanoma. This progress highlights the huge clinical potential of this treatment modality, and the focus is now combining these agents with conventional anti-cancer treatments or agents that enhance viral replication, and thereby oncolysis, in the tumour microenvironment. We evaluated the combination of reovirus with rapamycin in B16F10 cell, a murine model of malignant melanoma, based on potential mechanisms by which mTOR inhibitors might enhance viral oncolysis. Rapamycin was not immunomodulatory in that it had no effect on the generation of an anti-reovirus neutralising antibody response in C57/black 6 mice. The cell cycle effects of reovirus (increase G0/G1 fraction) were unaffected by concomitant or sequential exposure of rapamycin, However, rapamycin attenuated viral replication if given prior or concomitantly with reovirus and similarly reduced reovirus-induced apoptotic cell death annexin V/PI and caspase 3/7 activation studies. We found clear evidence of synergistic antitumour effects of the combination both in vitro and in vivo, which was sequence dependent only in the in vitro setting. In conclusion, we have demonstrated synergistic anti-tumour efficacy of reovirus and rapamycin combination.
Combination herpes simplex virus (HSV) oncolytic virotherapy and BRAF inhibitors (BRAFi) represent promising immunogenic treatments for BRAF mutant melanoma, but an improved understanding of the immunobiology of combinations is needed to improve on the benefit of immune checkpoint inhibitors (ICI). Using a BRAF -driven murine melanoma model, we tested the immunogenicity of HSV/BRAFi in immunocompetent C57BL mice. In addition to standard FACS analysis, we used the 'Timer of Cell Kinetics and Activity' system, which can analyze the temporal dynamics of different T cell subsets. This immune data was used to inform the selection of ICI for triple combination therapy, the effects of which were then further characterized using transcriptomics. Adding BRAFi treatment to HSV improved anti-tumor effects in vivo but not in vitro. Immune characterization showed HSV or dual therapy led to fewer intratumoral Treg, although with a more activated phenotype, together with more effector CD8 +T cells. Tocky analysis further showed that HSV/BRAFi dual treatment reduced the Tocky signal (reflecting engagement with cognate antigen), in both Treg and conventional subsets of CD4+, but not in CD8 +cells. However, a higher percentage of Treg than of conventional CD4 +maintained frequent engagement with antigens on treatment, reflecting a predominance of suppressive over effector function within the CD4 +compartment. The only T cell subset which correlated with a reduction in tumor growth was within Tocky signal positive conventional CD4+, supporting their therapeutic role. Targeting CD25 high, antigen-engaged Treg with a depleting anti-CD25 ICI, achieved complete cures in 100% of mice with triple therapy. Transcriptomic analysis confirmed reduction in Foxp3 on addition of anti-CD25 to HSV/BRAFi, as well as increases in expression of genes reflecting interferon signaling and cytotoxic activity. Combination HSV/BRAFi is an immunogenic therapy for BRAF mutant melanoma, but cannot fully control tumors. Dual therapy results in changes in T cell dynamics within tumors, with relatively maintained antigen signaling in Treg compared with conv CD4+. Antigen-engaged CD4 +effectors correlate with tumor growth control, and depletion of Treg by addition of an anti-CD25 ICI, releasing suppression of conventional CD4 +effectors by Treg, enhances survival and activates immune signaling within tumors.
The HOX genes are a family of closely related transcription factors that help to define the identity of cells and tissues during embryonic development and which are also frequently deregulated in a number of malignancies, including breast cancer. While relatively little is known about the roles that individual HOX genes play in cancer, it is however clear that these roles can be both contradictory, with some members acting as oncogenes and some as tumor suppressors, and also redundant, with several genes essentially having the same function. Here, we have attempted to address this complexity using the HXR9 peptide to target the interaction between HOX proteins and PBX, a second transcription factor that serves as a common co-factor for many HOX proteins. We show that HXR9 causes apoptosis in a number of breast cancer-derived cell lines and that sensitivity to HXR9 is directly related to the averaged expression of HOX genes HOXB1 through to HOXB9, providing a potential biomarker to predict the sensitivity of breast tumors to HXR9 or its derivatives. Measuring the expression of HOX genes HOXB1-HOXB9 in primary tumors revealed that a subset of tumors show highly elevated expression indicating that these might be potentially very sensitive to killing by HXR9. Furthermore, we show that while HXR9 blocks the oncogenic activity of HOX genes, it does not affect the known tumor-suppressor properties of a subset of HOX genes in breast cancer.
In pre-clinical models, the only two chemotherapy drugs which have been demonstrated to directly reduce the number of myeloid-derived suppressor cells (MDSCs) are gemcitabine and 5-fluorouracil. Here we analyze the dynamics of MDSCs, phenotyped as Lin-DR-CD11b+, in patients with advanced pancreatic cancer receiving the combination of gemcitabine and capecitabine, a 5-FU pro-drug. We found no evidence that gemcitabine and capecitabine directly reduce MDSC% in patients. Gemcitabine and capecitabine reduced MDSCs in 42 % of patients (n = 19) and MDSC% fell in only 3/9 patients with above-median baseline MDSCs. In 5/8 patients with minimal tumour volume change on treatment, the MDSC% went up: increases in MDSC% in these patients appeared to correlate with sustained cancer-related inflammatory cytokine upregulation. In a separate cohort of 21 patients treated with gemcitabine and capecitabine together with concurrently administered GV1001 vaccine with adjuvant GM-CSF, the MDSC% fell in 18/21 patients and there was a significant difference in the trajectory of MDSCs between those receiving GV1001 and GM-CSF in combination with chemotherapy and those receiving chemotherapy alone. Thus, there was no evidence that the addition of low-dose adjuvant GM-CSF increased Lin-DR-CD11b+ MDSC in patients receiving combination chemoimmunotherapy. 9/21 patients developed an immune response to GV1001 and the MDSCs fell in 8 of these 9 patients, 6 of whom had above-median pre-vaccination MDSC levels. A high pre-vaccination MDSC% does not preclude the development of immunity to a tumour-associated antigen.
Genetic risk scores were used as unconfounded instruments for specific lipid traits (Mendelian randomization) to assess whether circulating lipids causally influence prostate cancer risk. Data from 22,249 prostate cancer cases and 22,133 controls from 22 studies within the international PRACTICAL consortium were analyzed. Allele scores based on single nucleotide polymorphisms (SNPs) previously reported to be uniquely associated with each of low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglyceride (TG) levels, were first validated in an independent dataset, and then entered into logistic regression models to estimate the presence (and direction) of any causal effect of each lipid trait on prostate cancer risk. There was weak evidence for an association between the LDL genetic score and cancer grade: the odds ratio (OR) per genetically instrumented standard deviation (SD) in LDL, comparing high- (≥7 Gleason score) versus low-grade (
Multigene assays can provide insight into key biological processes and prognostic information to guide development and selection of adjuvant cancer therapy. We report a comprehensive genomic and transcriptomic analysis of tumor samples from 171 patients at high risk for recurrent renal cell carcinoma post nephrectomy from the S-TRAC trial (NCT00375674). We identify gene expression signatures, including STRAC11 (derived from the sunitinib-treated population). The overlap in key elements captured in these gene expression signatures, which include genes representative of the tumor stroma microenvironment, regulatory T cell, and myeloid cells, suggests they are likely to be both prognostic and predictive of the anti-angiogenic effect in the adjuvant setting. These signatures also point to the identification of potential therapeutic targets for development in adjuvant renal cell carcinoma, such as MERTK and TDO2. Finally, our findings suggest that while anti-angiogenic adjuvant therapy might be important, it may not be sufficient to prevent recurrence and that other factors such as immune response and tumor environment may be of greater importance. Based on the S-TRAC results, sunitinib is approved as adjuvant treatment for adult patients at high risk of recurrent RCC following nephrectomy. Here, the authors report the results of an integrated multi-omics tumor analysis of 171 patients from the trial and identify specific molecular subtypes as well as potential new targets.
Prostate cancers are considered “cold” tumors characterized by minimal T cell infiltrates, absence of a type I interferon (IFN) signature, and the presence of immunosuppressive cells. This non-inflamed phenotype is likely responsible for the lack of sensitivity of prostate cancer patients to immune checkpoint blockade (ICB) therapy. Oncolytic virus therapy can potentially overcome this resistance to immunotherapy in prostate cancers by transforming cold tumors into “hot,” immune cell-infiltrated tumors. We investigated whether the combination of intratumoral oncolytic reovirus, followed by targeted blockade of Programmed cell death protein 1 (PD-1) checkpoint inhibition and/or the immunomodulatory CD73/Adenosine system can enhance anti-tumor immunity. Treatment of subcutaneous TRAMP-C2 prostate tumors with combined intratumoral reovirus and anti-PD-1 or anti-CD73 antibody significantly enhanced survival of mice compared with reovirus or either antibody therapy alone. Only combination therapy led to rejection of pre-established tumors and protection from tumor re-challenge. This therapeutic effect was dependent on CD4 + T cells and natural killer (NK) cells. NanoString immune profiling of tumors confirmed that reovirus increased tumor immune cell infiltration and revealed an upregulation of the immune-regulatory receptor, B- and T-lymphocyte attenuator (BTLA). This expression of BTLA on innate antigen-presenting cells (APCs) and its ligand, Herpesvirus entry mediator (HVEM), on T cells from reovirus-infected tumors was in keeping with a role for the HVEM-BTLA pathway in promoting the potent anti-tumor memory response observed. Immunotherapy in prostate cancer is limited because of a lack of immune cells within the tumor. Annels et al. used oncolytic viruses to recruit immune cells into the tumor and showed that in combination with checkpoint inhibitors, which take the brake off of the immune system, established tumors were rejected.
From a therapeutic perspective, the bourgeoning literature on Th17 cells should allow us to decide whether to rationally pursue the manipulation of Th17 cells in cancer. The purpose of this review is to attempt a synthesis of a number of contradictory conclusions as to the role that these cells are playing in the process of tumourigenesis in order to provide guidance as to whether our current understanding is sufficient to safely pursue Th17-targeted therapy in cancer at this time. Th17 cells are a highly plastic population and the cytokine drivers for Th17 cell generation and skewing will vary between various cancers and importantly between different sites of tumour involvement in any individual patient. The net impact of the pro-angiogenic IL-17 produced not only by Th17 cells but by other cells particularly macrophages and the anti-tumour effects of Th1/Th17 cells will in turn be determined by the complex interplay of diverse chemokines and cytokines in any tumour microenvironment. Th17 cells that fail to home to tumours may be immunosuppressive. The complexity of IL-17 and Th17 dynamics makes easy prediction of the effects of either enhancing or suppressing Th17 cell differentiation in cancer problematic.
Reovirus exploits aberrant signalling downstream of Ras to mediate tumor-specific oncolysis. Since ~90% squamous cell carcinomas of the head and neck (SCCHN) over-express EGFR and SCCHN cell lines are sensitive to oncolytic reovirus, we conducted a detailed analysis of the effects of reovirus in 15 head and neck cancer cell lines. Both pre- and post-entry events were studied in an attempt to define biomarkers predictive of sensitivity/resistance to reovirus. In particular, we analysed the role of EGFR/Ras signalling in determining virus-mediated cytotoxicity in SCCHN.
Background: Prostate cancer is a common cancer worldwide with no established modifiable lifestyle factors to guide prevention. The associations between polyunsaturated fatty acids (PUFAs) and prostate cancer risk have been inconsistent. Using Mendelian randomisation, we evaluated associations between PUFAs and prostate cancer risk. Methods: We used individual-level data from a consortium of 22 721 cases and 23 034 controls of European ancestry. Externally-weighted PUFA-specific polygenic risk scores (wPRSs), with explanatory variation ranging from 0.65 to 33.07%, were constructed and used to evaluate associations with prostate cancer risk per one standard deviation (s.d.) increase in genetically-predicted plasma PUFA levels using multivariable-adjusted unconditional logistic regression. Results: No overall association was observed between the genetically-predicted PUFAs evaluated in this study and prostate cancer risk. However, risk reductions were observed for short-chain PUFAs, linoleic (ORLA=0.95, 95%CI=0.92, 0.98) and α-linolenic acids (ORALA=0.96, 95%CI=0.93, 0.98), among men
Immune checkpoint inhibitors, including those targeting programmed cell death protein 1 (PD-1), are reshaping cancer therapeutic strategies. Evidence suggests, however, that tumor response and patient survival are determined by tumor programmed death-ligand 1 (PD-L1) expression. We hypothesized that preconditioning of the tumor immune microenvironment using targeted, virus-mediated interferon (IFN) stimulation, would upregulate tumor PD-L1 protein expression and increase cytotoxic T cell infiltration, improving the efficacy of subsequent checkpoint blockade. Oncolytic viruses (OVs) represent a promising form of cancer immunotherapy. For brain tumors, almost all studies to date have used direct intralesional injection of OV, because of the largely untested belief that intravenous (i.v.) administration will not deliver virus to this site. Here we show, in a window-of-opportunity clinical study, that i.v. infusion of oncolytic human Orthoreovirus (referred to herein as reovirus), leads to infection of tumor cells subsequently resected as part of standard clinical care, both in high-grade glioma (HGG) and in brain metastases, and increases cytotoxic T cell tumor infiltration relative to patients not treated with virus. We further show that reovirus upregulates IFN-regulated gene expression, as well as the PD-1/PD-L1 axis in tumors, via an IFN-mediated mechanism. Finally, we show that addition of PD-1 blockade to reovirus enhances systemic therapy in a preclinical glioma model. These results support the development of combined systemic immunovirotherapy strategies for the treatment of both primary and secondary tumors in the brain.
Controversy surrounds the use of PSA as a biomarker for prostate cancer detection, leaving an unmet need for a novel biomarker in this setting; urinary EN2 may identify individuals with clinically relevant prostate cancer. Male BRCA1 and BRCA2 mutation carriers are at increased risk of clinically significant prostate cancer and may benefit from screening. Urine samples from 413 BRCA1 and BRCA2 mutation carriers and controls were evaluated. Subjects underwent annual PSA screening with diagnostic biopsy triggered by PSA > 3.0 ng/ml; 21 men were diagnosed with prostate cancer. Urinary EN2 levels were measured by ELISA and had a sensitivity of 66.7% and specificity of 89.3% for cancer detection. There was no statistically significant difference in EN2 levels according to genetic status or Gleason score. Urinary EN2 may be useful as a non-invasive early biomarker for prostate cancer detection in genetically high-risk individuals.
Reovirus is a promising oncolytic virus, acting by both direct and immune-mediated mechanisms, although its potential may be limited by inactivation after systemic delivery. Our study addressed whether systemically delivered reovirus might be shielded from neutralising antibodies by cell carriage and whether virus-loaded blood or hepatic innate immune effector cells become activated to kill colorectal cancer cells metastatic to the liver in human systems. We found that reovirus was directly cytotoxic against tumour cells but not against fresh hepatocytes. Although direct tumour cell killing by neat virus was significantly reduced in the presence of neutralising serum, reovirus was protected when loaded onto peripheral blood mononuclear cells, which may carry virus after intravenous administration in patients. As well as handing off virus for direct oncolytic killing, natural killer (NK) cells within reovirus-treated blood mononuclear cells were stimulated to kill tumour targets, but not normal hepatocytes, in a Type I interferon-dependent manner. Similarly, NK cells within liver mononuclear cells became selectively cytotoxic towards tumour cells when activated by reovirus. Hence, intravenous reovirus may evade neutralisation by serum via binding to circulating mononuclear cells, and this blood cell carriage has the potential to investigate both direct and innate immune-mediated therapy against human colorectal or other cancers metastatic to the liver.
Purpose. Nonmuscle invasive bladder cancer (BCa) has a high recurrence rate requiring lifelong surveillance. Urinary biomarkers are promising as simple alternatives to cystoscopy for the diagnosis of recurrent bladder cancer. However, no single marker can achieve the required accuracy. The purpose of this study was to select a multiparameter panel, comprising urinary biomarkers and clinical parameters, for BCa recurrence diagnosis. Experimental Design. Candidate biomarkers were measured in urine samples of BCa patients with recurrence and BCa patients without recurrence. A multiplatform strategy was used for marker quantification comprising a multiplexed microarray and an automated platform for ELISA analysis. A multivariate statistical analysis combined the results from both platforms with the collected clinical data. Results. The best performing combination of biomarkers and clinical parameters achieved an AUC value of 0.91, showing better performance than individual parameters. This panel comprises six biomarkers (cadherin-1, IL-8, ErbB2, IL-6, EN2, and VEGF-A) and three clinical parameters (number of past recurrences, number of BCG therapies, and stage at time of diagnosis). Conclusions. The multiparameter panel could be a useful noninvasive tool for BCa surveillance and potentially impact the clinical management of this disease. Validation of results in an independent cohort is warranted.
Effective cancer immunotherapy requires the release of a broad spectrum of tumor antigens in the context of potent immune activation. We show here that a cDNA library of normal tissue, expressed from a highly immunogenic viral platform, cures established tumors of the same histological type from which the cDNA library was derived. Immune escape occurred with suboptimal vaccination, but tumor cells that escaped the immune pressure were readily treated by second-line virus-based immunotherapy. This approach has several major advantages. Use of the cDNA library leads to presentation of a broad repertoire of (undefined) tumor-associated antigens, which reduces emergence of treatment-resistant variants and also permits rational, combined-modality approaches in the clinic. Finally, the viral vectors can be delivered systemically, without the need for tumor targeting, and are amenable to clinical-grade production. Therefore, virus-expressed cDNA libraries represent a novel paradigm for cancer treatment addressing many of the key issues that have undermined the efficacy of immuno- and virotherapy to date.
Background: Epidemiological studies have observed a positive association between an earlier age at sexual development and prostate cancer, but markers of sexual maturation in boys are imprecise and observational estimates are likely to suffer from a degree of uncontrolled confounding. To obtain causal estimates, we examined the role of pubertal development in prostate cancer using genetic polymorphisms associated with Tanner stage in adolescent boys in a Mendelian randomization (MR) approach. Methods: We derived a weighted genetic risk score for pubertal development, combining 13 SNPs associated with male Tanner stage. A higher score indicated a later puberty onset. We examined the association of this score with prostate cancer risk, stage and grade in the UK-based ProtecT case-control study (n = 2,927), and used the PRACTICAL consortium (n = 43,737) as a replication sample. Results: In ProtecT, the puberty genetic score was inversely associated with prostate cancer grade (odds ratio (OR) of high- vs. low-grade cancer, per tertile of the score: 0.76; 95 % CI, 0.64–0.89). In an instrumental variable estimation of the causal OR, later physical development in adolescence (equivalent to a difference of one Tanner stage between pubertal boys of the same age) was associated with a 77 % (95 % CI, 43–91 %) reduced odds of high Gleason prostate cancer. In PRACTICAL, the puberty genetic score was associated with prostate cancer stage (OR of advanced vs. localized cancer, per tertile: 0.95; 95 % CI, 0.91–1.00) and prostate cancer-specific mortality (hazard ratio amongst cases, per tertile: 0.94; 95 % CI, 0.90–0.98), but not with disease grade. Conclusions: Older age at sexual maturation is causally linked to a reduced risk of later prostate cancer, especially aggressive disease.
Glioblastoma multiforme (GBM) is the most common high-grade malignant brain tumour in adults and arises from the glial cells in the brain. The prognosis of treated GBM remains very poor with 5-year survival rates of 5%, a figure which has not improved over the last few decades. Currently, there is a modest 14-month overall median survival in patients undergoing maximum safe resection plus adjuvant chemoradiotherapy. HOX gene dysregulation is now a widely recognised feature of many malignancies. In this study we have focused on HOX gene dysregulation in GBM as a potential therapeutic target in a disease with high unmet need. We show significant dysregulation of these developmentally crucial genes and specifically that HOX genes A9, A10, C4 and D9 are strong candidates for biomarkers and treatment targets for GBM and GBM cancer stem cells. We evaluated a next generation therapeutic peptide, HTL-001, capable of targeting HOX gene over-expression in GBM by disrupting the interaction between HOX proteins and their co-factor, PBX. HTL-001 induced both caspase-dependent and -independent apoptosis in GBM cell lines. In vivo biodistribution studies confirmed that the peptide was able to cross the blood brain barrier. Systemic delivery of HTL-001 resulted in improved control of subcutaneous murine and human xenograft tumours and improved survival in a murine orthotopic model.
Almost 50,000 men in the United Kingdom (UK) are diagnosed each year with prostate cancer (PCa). Secondary referrals for investigations rely on serum prostate-specific antigen (PSA) levels and digital rectal examination. However, both tests lack sensitivity and specificity, resulting in unnecessary referrals to secondary care for costly and invasive biopsies. Serum samples and clinical information were collected from = 125 age-matched patients ( = 61 non-PCa and = 64 PCa) and analyzed using Biochip Array Technology on high-sensitivity cytokine array I (IL-2, IL-4, IL-6, IL-8, IL-10, IL-1α, IL-1β, TNFα, MCP-1, INFγ, EGF, and VEGF), cerebral array II (CRP, D-dimer, neuron-specific enolase, and sTNFR1), and tumor PSA oncology array (fPSA, tPSA, and CEA). The data showed that 11/19 (68.8%) markers were significantly different between the non-PCa and the PCa patients. A combination of EGF, log IL-8, log MCP-1, and log tPSA significantly improved the predictive potential of tPSA alone to identify patients with PCa (DeLong,< 0.001). This marker combination had an increased area under the receiver operator characteristic (0.860 . 0.700), sensitivity (78.7 . 68.9%), specificity (76.5 . 67.2%), PPV (76.2 . 66.7%), and NPV (79.0 . 69.4%) compared with tPSA. The novel combination of serum markers identified in this study could be employed to help triage patients into "low-" and "high-risk" categories, allowing general practitioners to improve the management of patients in primary care settings and potentially reducing the number of referrals for unnecessary, invasive, and costly treatments.
Metastatic neuroendocrine prostate cancer (NEPC) is a highly aggressive disease, whose incidence is rising. Long noncoding RNAs (lncRNAs) represent a large family of disease- and tissue-specific transcripts, most of which are still functionally uncharacterized. Thus, we set out to identify the highly conserved lncRNAs that play a central role in NEPC pathogenesis. To this end, we performed transcriptomic analyses of donor-matched patient-derived xenograft models (PDXs) with immunohistologic features of prostate adenocarcinoma (AR /PSA ) or NEPC (AR /SYN /CHGA ) and through differential expression analyses identified lncRNAs that were upregulated upon neuroendocrine transdifferentiation. These genes were prioritized for functional assessment based on the level of conservation in vertebrates. Here, LINC00261 emerged as the top gene with over 3229-fold upregulation in NEPC. Consistently, LINC00261 expression was significantly upregulated in NEPC specimens in multiple patient cohorts. Knockdown of LINC00261 in PC-3 cells dramatically attenuated its proliferative and metastatic abilities, which are explained by parallel downregulation of CBX2 and FOXA2 through distinct molecular mechanisms. In the cell cytoplasm, LINC00261 binds to and sequesters miR-8485 from targeting the CBX2 mRNA, while inside the nucleus, LINC00261 functions as a transcriptional scaffold to induce SMAD-driven expression of the FOXA2 gene. For the first time, these results demonstrate hyperactivation of the LINC00261-CBX2-FOXA2 axes in NEPC to drive proliferation and metastasis, and that LINC00261 may be utilized as a therapeutic target and a biomarker for this incurable disease.
It is now well-recognized that the tumor microenvironment (TME) is not only a key regulator of cancer progression but also plays a crucial role in cancer treatment responses. Recently, several high-profile publications have demonstrated the importance of particular immune parameters and cell types that dictate responsiveness to immunotherapies. With this increased understanding of TME-mediated therapy, approaches that increase therapeutic efficacy by remodeling the TME are actively being pursued. A classic example of this, in practice by urologists for over 40 years, is the manipulation of the bladder microenvironment for the treatment of non-muscle invasive bladder cancer (NMIBC) by instillation of intravesical bacillus Calmette-Guerin (BCG). The success of BCG treatment is thought to be due to its ability to induce a massive influx of Th1-polarized inflammatory cells, production of Th1 inflammatory cytokines and the generation of tumor-targeted Th1-mediated cytotoxic responses. Whilst BCG immunotherapy is currently the best treatment for NMIBC, similar to 30% of patients show no response to this treatment. Here we present a review highlighting a variety of promising alternative immunotherapies being developed that remodel the bladder tumor microenvironment. These include (1) the use of oncolytic viruses which selectively replicate within cancer cells whilst also modifying the immunological components of the TME, (2) manipulation of the bladder microbiome to augment the response to BCG or other immunotherapies (3) utilizing Toll-like Receptor agonists as anti-tumor agents due to their potent stimulation of innate and adaptive immunity and (4) the growing recognition that immunotherapeutic strategies that will have the largest impact on patients may require multiple therapeutic approaches combined together. The accumulating knowledge on TME remodeling holds promise for providing an alternative therapy for patients with BCG-unresponsive NMIBC.
Improvements in cancer survival mean that long-term toxicities, which contribute to the morbidity of cancer survivorship, are being increasingly recognized. Late adverse effects (LAEs) in normal tissues after radiotherapy (RT) are characterized by vascular dysfunction and fibrosis causing volume loss and tissue contracture, for example, in the free flaps used for immediate breast reconstruction after mastectomy. We evaluated the efficacy of lentivirally delivered superoxide dismutase 2 (SOD2) overexpression and connective tissue growth factor (CTGF) knockdown by short hairpin RNA in reducing the severity of LAEs in an animal model of free flap LAEs. Vectors were delivered by intra-arterial injection, ex vivo, to target the vascular compartment. LVSOD2 and LVshCTGF monotherapy before irradiation resulted in preservation of flap volume or reduction in skin contracture, respectively. Flaps transduced with combination therapy experienced improvements in both volume loss and skin contracture. Both therapies reduced the fibrotic burden after irradiation. LAEs were associated with impaired vascular perfusion, loss of endothelial permeability, and stromal hypoxia, which were all reversed in the treatment model. Using a tumor recurrence model, we showed that SOD2 overexpression in normal tissues did not compromise the efficacy of RT against tumor cells but appeared to enhance it. LVSOD2 and LVshCTGF combination therapy by targeted, intravascular delivery reduced LAE severities in normal tissues without compromising the efficacy of RT and warrants translational evaluation as a free flap–targeted gene therapy.
Background The most important insights into mechanisms of tumour rejection, and how these could be exploited therapeutically, is likely to come from patients displaying the best responses. Those individuals with complete and sustained antitumour responses, without maintenance therapy, will provide the best evidence of genuine disease modification. Despite much speculation as to how these exceptional responses are generated there is increasing evidence for an immune basis which may be influenced by the tumour microbiome underlying the mechanism for sustained tumour rejection. Methods To focus on individuals with complete and sustained metastatic disease resolution, we designed a pilot study, the Continuum Long-Term Survivor study, to evaluate patients with the best outcomes, where disease modification may have occurred. The study targeted only those patients (n=50) with a sustained (>5 years) complete clearance of metastatic cancers, without requiring maintenance therapy. Matched controls comprised patients unable to generate an initial response, or those who relapsed within 12 months. DNA extracted from tumour samples was analyzed by 16S BENCHMARK™ microbial amplicon sequencing (Diversigen) to profile the tumour microbiome, whilst the microbial composition of stool samples was determined using BoosterShot Shotgun Sequencing. In parallel mRNA expression from the tumour tissue was evaluated using NanoString’s PanCancer IO360 gene expression panel. From a homogeneous subgroup of bowel cancer long-term survivors and their matched controls, multiplex IHC using a panel of 8 immune markers to identify tertiary lymphoid structures (TLS) was performed on the tumour tissues and imaged using a PhenoImager (AkoyaBiosciences). Results Results will be presented comparing tumour and gut-derived microbial species diversity between long-term vs. short-term survivor matched controls using alpha diversity estimates as well as differential abundance analysis. This will define the microbial species that are more likely to be associated with long-term survivorship. Characterization of the immune gene transcriptional patterns within the tumour microenvironment (TME) from long-term survivors vs controls will also be reported along with any observed differences from the multiplex IHC analysis of immune infiltrates in corresponding patient tissue. To explore any connections of the tumour-microbiome on the TME, an integrated analysis of the microbiome and tumour immune transcriptome will be presented. Conclusions This study will reveal whether changes in TME influenced by the tumour microbiota may be important factors associated with long-term survivorship. Understanding the precise mechanisms of total tumour rejection in patients, and their evaluation may be game-changing in terms of design of new molecular, biological and immune therapies. Ethics Approval This study was approved by the University of Surrey Ethics Board; approval number 266581.
We undertook a comprehensive analysis of circulating myeloid-derived suppressor cells (MDSCs) and T regulatory cells (Tregs) in pancreatic, esophageal and gastric cancer patients and investigated whether MDSCs are an independent prognostic factor for survival. We evaluated a series of plasma cytokines and in particular re-evaluated the Th2 cytokine interleukin-13 (IL-13). Peripheral blood was collected from 131 cancer patients (46 pancreatic, 60 esophageal and 25 gastric) and 54 healthy controls. PBMC were harvested with subsequent flow cytometric analysis of MDSC (HLADR(-) Lin1(low/-) CD33(+) CD11b(+)) and Treg (CD4(+) CD25(+) CD127(low/-) FoxP3(+)) percentages. Plasma IL-2, IL-4, IL-5, IL-6, IL-10, IL-12 (p70), IL-13, IL-17, G-CSF, IFN-γ, TNF-α and VEGF levels were analyzed by the Bio-Plex cytokine assay. Plasma arginase I levels were analyzed by ELISA. MDSCs and Tregs were statistically significantly elevated in pancreatic, esophageal and gastric cancer compared with controls, and MDSC numbers correlated with Treg levels. Increasing MDSC percentage was associated with increased risk of death, and in a multivariate analysis, MDSC level was an independent prognostic factor for survival. A unit increase in MDSC percentage was associated with a 22% increased risk of death (hazard ratio 1.22, 95% confidence interval 1.06-1.41). Arginase I levels were also statistically significantly elevated in upper gastrointestinal cancer patients compared with controls. There was Th2 skewing for cytokine production in all three diseases, and importantly there were significant elevations of the pivotal Th2 cytokine interleukin-13, an increase that correlated with MDSC levels.
The homeobox (HOX) genes are a highly conserved family of homeodomain-containing transcription factors that specify cell identity in early development and, subsequently, in a number of adult processes including hematopoiesis. The dysregulation of HOX genes is associated with a number of malignancies including acute myeloid leukemia (AML) and acute lymphoid leukemia (ALL), where they have been shown to support the immortalization of leukemic cells both as chimeric partners in fusion genes and when overexpressed in their wild-type form. This review covers our current understanding of the role of HOX genes in normal hematopoiesis, AML and ALL, with particular emphasis on the similarities and differences of HOX function in these contexts, their hematopoietic downstream gene targets and implications for therapy. © 2013 Macmillan Publishers Limited All rights reserved.
The HOX genes are a highly conserved group of transcription factors that have key roles in early development, but which are also highly expressed in most cancers. Many studies have found strong associative relationships between the expression of individual HOX genes in tumours and clinical parameters including survival. For the majority of HOX genes, high tumour expression levels seem to be associated with a worse outcome for patients, and in some cases, this has been shown to result from the activation of pro-oncogenic genes and pathways. However, there are also many studies that indicate a tumour suppressor role for some HOX genes, sometimes with conclusions that contradict earlier work. In this review, we have attempted to clarify the role of HOX genes in cancer by focusing on their downstream targets as identified in studies that provide experimental evidence for their activation or repression. On this basis, the majority of HOX genes would appear to have a pro-oncogenic function, with the notable exception of HOXD10, which acts exclusively as a tumour suppressor. HOX proteins regulate a wide range of target genes involved in metastasis, cell death, proliferation and angiogenesis, and activate key cell signalling pathways. Furthermore, for some functionally related targets, this regulation is achieved by a relatively small subgroup of HOX genes.
BackgroundOncolytic reovirus therapy for cancer induces a typical antiviral response to this RNA virus, including neutralizing antibodies. Concomitant treatment with cytotoxic chemotherapies has been hypothesized to improve the therapeutic potential of the virus. Chemotherapy side effects can include immunosuppression, which may slow the rate of the antiviral antibody response, as well as potentially make the patient more vulnerable to viral infection.MethodReovirus neutralizing antibody data were aggregated from separate phase I clinical trials of reovirus administered as a single agent or in combination with gemcitabine, docetaxel, carboplatin and paclitaxel doublet or cyclophosphamide. In addition, the kinetics of individual antibody isotypes were profiled in sera collected in these trials.ResultsThese data demonstrate preserved antiviral antibody responses, with only moderately reduced kinetics with some drugs, most notably gemcitabine. All patients ultimately produced an effective neutralizing antibody response.ConclusionPatients’ responses to infection by reovirus are largely unaffected by the concomitant drug treatments tested, providing confidence that RNA viral treatment or infection is compatible with standard of care treatments.
APOBEC3B, an anti-viral cytidine deaminase which induces DNA mutations, has been implicated as a mediator of cancer evolution and therapeutic resistance. Mutational plasticity also drives generation of neoepitopes, which prime anti-tumor T cells. Here, we show that overexpression of APOBEC3B in tumors increases resistance to chemotherapy, but simultaneously heightens sensitivity to immune checkpoint blockade in a murine model of melanoma. However, in the vaccine setting, APOBEC3B-mediated mutations reproducibly generate heteroclitic neoepitopes in vaccine cells which activate de novo T cell responses. These cross react against parental, unmodified tumors and lead to a high rate of cures in both subcutaneous and intra-cranial tumor models. Heteroclitic Epitope Activated Therapy (HEAT) dispenses with the need to identify patient specific neoepitopes and tumor reactive T cells ex vivo. Thus, actively driving a high mutational load in tumor cell vaccines increases their immunogenicity to drive anti-tumor therapy in combination with immune checkpoint blockade.
OBJECTIVE: HOX genes are vital for all aspects of mammalian growth and differentiation, and their dysregulated expression is related to ovarian carcinogenesis. The aim of the current study was to establish the prognostic value of HOX dysregulation as well as its role in platinum resistance. The potential to target HOX proteins through the HOX/PBX interaction was also explored in the context of platinum resistance. METHODS: HOX gene expression was determined in ovarian cancer cell lines and primary EOCs, and compared to expression in normal ovarian epithelium and fallopian tube tissue samples. Statistical analysis included one way ANOVA and t-tests, using statistical software R and GraphPad. RESULTS: 30 of the 39 HOX genes were overexpressed in high grade serous EOC compared to normal tissue, most significant being HOXA3, A9, B13 and C10. We detected a molecular HOX gene-signature that predicted poor outcome: overexpression of HOXB4 and HOXB9 was identified in high grade serous cell lines after platinum resistance developed. Targeting the HOX/PBX dimer with the the HXR9 peptide enhanced the cytotoxicity of cisplatin in platinum-resistant ovarian cancer.CONCLUSIONS: HOX genes are highly dysregulated in ovarian cancer. High expression of HOXA13, B6, C13, D1 and D13 is predictive of poor clinical outcome. Targeting the HOX/PBX dimer in platinum–resistant cancer represents a new therapeutic option that should be further developed and tested in clinical trials.
The HOX genes are a family of homeodomain-containing transcription factors that determine cellular identity during development and which are subsequently re-expressed in many types of cancer. Some recent studies have shown that HOX genes may have key roles both in pancreatic development and in adult diseases of the pancreas, including cancer. In this review we consider recent advances in elucidating the role of HOX genes in these processes, how they may connect early developmental events to subsequent adult disease, and their potential both as diagnostic markers and therapeutic targets.
We determined the effect of sample size on performance of polygenic hazard score (PHS) models in prostate cancer. Age and genotypes were obtained for 40,861 men from the PRACTICAL consortium. The dataset included 201,590 SNPs per subject, and was split into training and testing sets. Established-SNP models considered 65 SNPs that had been previously associated with prostate cancer. Discovery-SNP models used stepwise selection to identify new SNPs. The performance of each PHS model was calculated for random sizes of the training set. The performance of a representative Established-SNP model was estimated for random sizes of the testing set. Mean HR 98/50 (hazard ratio of top 2% to average in test set) of the Established-SNP model increased from 1.73 [95% CI: 1.69–1.77] to 2.41 [2.40–2.43] when the number of training samples was increased from 1 thousand to 30 thousand. Corresponding HR 98/50 of the Discovery-SNP model increased from 1.05 [0.93–1.18] to 2.19 [2.16–2.23]. HR 98/50 of a representative Established-SNP model using testing set sample sizes of 0.6 thousand and 6 thousand observations were 1.78 [1.70–1.85] and 1.73 [1.71–1.76], respectively. We estimate that a study population of 20 thousand men is required to develop Discovery-SNP PHS models while 10 thousand men should be sufficient for Established-SNP models.
Background: Prostate cancer is a leading cause of cancer related death in men but its diagnosis is still complicated by the lack of a highly predictive biochemical marker. Here we show that the transcription factor Engrailed-2 is secreted from prostate tumours in a highly specific manner and is present in the urine of men with prostate cancer. Methods: Urine was collected under standardised conditions from men with prostate cancer, or with non-cancerous conditions of the prostate such as benign prostatic hypertrophy, or men who were found to have no prostate abnormalities after saturation biopsy. Results: Engrailed-2 protein was detected in the untreated, unconcentrated urine of 62% of men with prostate cancer, but only 3% of men with no prostatic abnormalities (n=258, p
Despite extensive efforts to identify a clinically useful diagnostic biomarker in prostate cancer, no new test has been approved by regulatory authorities. As a result, this unmet need has shifted to biomarkers that additionally indicate presence or absence of "significant" disease. EN2 is a homeodomain-containing transcription factor secreted by prostate cancer into the urine and can be detected by enzyme-linked immunoassay. EN2 may be an ideal biomarker because normal prostate tissue and benign prostatic hypertrophic cells do not secrete EN2. This review discusses the enormous potential of EN2 to address this unmet need and provide the urologist with a simple, inexpensive, and reliable prostate cancer biomarker.
What's known on the subject? and What does the study add? There are a lot of potential prostate cancer biomarkers being evaluated. All aim to improve on the sensitivity and specificity of PSA. EN2 was recently shown by our group to have better sensitivity and specificity than PSA. EN2 is a simple ELISA test and is not dependent on other parameters, even PSA, unlike all the other current biomarkers under evaluation. To date, no marker correlates with the amount of cancer present - the present study shows this positive correlation with EN2 in men undergoing prostatectomy. The potential utility of this work is that by knowing that the level of EN2 corresponds to the amount of cancer present, irrelevant of tumour grade and number of cancer foci, we can define an EN2 level corresponding to small cancers, which can then undergo surveillance. We are conducting a further study that is aimed at determining whether the levels of EN2 in urine can indicate 'significant' vs 'non-significant cancer' using the threshold of 0.5 mL cancer (after Epstein's work).
Androgen receptor targeted therapies for prostate cancer have serious limitations in advanced stages of the disease. While resistance to the FDA-approved enzalutamide is extensively documented, novel therapies based on epichlorohydrin scaffolds (EPI) are currently in clinical trials, but display suboptimal pharmacokinetics. Herein, we report the synthesis and biological characterisation of a novel class of compounds designed through covalently linking enzalutamide and EPI-001 through various triazole based linkers. The compounds display an 18 to 53 fold improvement in the cell killing potency towards C4-2b prostate cancer (PCa) cells compared to the gold standards of therapy, enzalutamide and EPI-001. The most promising compounds were proven to exhibit their toxicity exclusively through androgen receptor (AR) mediated pathways. This work sets the basis for the first class of hybrid AR inhibitors which successfully combine two drug moieties - EPI-001 and enzalutamide - into the same molecule.
Simple Summary This review summarizes the current literature related to the microbiome and pancreatic ductal adenocarcinoma (PDAC). The aim of this review is to explore the current role of the microbiome in the disease process, screening/diagnostics and to postulate the future role with regards to therapeutic strategies including chemotherapy, immunotherapy and surgery. We further explore the future of microbiome modulation (faecal microbiome transplants, bacterial consortiums, anti-microbials and probiotics), their applications and how we can improve the future of microbiome modulation in a bid to improve PDAC outcomes. Pancreatic ductal adenocarcinoma (PDAC) is expected to become the second most common cause of cancer death in the USA by 2030, yet progress continues to lag behind that of other cancers, with only 9% of patients surviving beyond 5 years. Long-term survivorship of PDAC and improving survival has, until recently, escaped our understanding. One recent frontier in the cancer field is the microbiome. The microbiome collectively refers to the extensive community of bacteria and fungi that colonise us. It is estimated that there is one to ten prokaryotic cells for each human somatic cell, yet, the significance of this community in health and disease has, until recently, been overlooked. This review examines the role of the microbiome in PDAC and how it may alter survival outcomes. We evaluate the possibility of employing microbiomic signatures as biomarkers of PDAC. Ultimately this review analyses whether the microbiome may be amenable to targeting and consequently altering the natural history of PDAC.
Persistent androgen receptor (AR) signalling is the main driver of prostate cancer (PCa). Truncated isoforms of the AR called androgen receptor variants (AR-Vs) lacking the ligand binding domain often emerge during treatment resistance against AR pathway inhibitors such as Enzalutamide. This review discusses how AR-Vs drive a more aggressive form of PCa through the regulation of some of their target genes involved in oncogenic pathways, enabling disease progression. There is a pressing need for the development of a new generation of AR inhibitors which can repress the activity of both the full-length AR and AR-Vs, for which the knowledge of differentially expressed target genes will allow evaluation of inhibition efficacy. This review provides a detailed account of the most common variant, AR-V7, the AR-V7 regulated genes which have been experimentally validated, endeavours to understand their relevance in aggressive AR-V driven PCa and discusses the utility of the downstream protein products as potential drug targets for PCa treatment.
The objective is to develop a multivariable risk model for the non-invasive detection of prostate cancer prior to biopsy by integrating information from clinically available parameters, Engrailed-2 (EN2) whole-urine protein levels and data from urinary cell-free RNA. Post-digital-rectal examination urine samples collected as part of the Movember Global Action Plan 1 study which has been analysed for both cell-free-RNA and EN2 protein levels were chosen to be integrated with clinical parameters ( = 207). A previously described robust feature selection framework incorporating bootstrap resampling and permutation was applied to the data to generate an optimal feature set for use in Random Forest models for prediction. The fully integrated model was named ExoGrail, and the out-of-bag predictions were used to evaluate the diagnostic potential of the risk model. ExoGrail risk (range 0-1) was able to determine the outcome of an initial trans-rectal ultrasound guided (TRUS) biopsy more accurately than clinical standards of care, predicting the presence of any cancer with an area under the receiver operator curve (AUC) = 0.89 (95% confidence interval(CI): 0.85-0.94), and discriminating more aggressive Gleason ≥ 3 + 4 disease returning an AUC = 0.84 (95% CI: 0.78-0.89). The likelihood of more aggressive disease being detected significantly increased as ExoGrail risk score increased (Odds Ratio (OR) = 2.21 per 0.1 ExoGrail increase, 95% CI: 1.91-2.59). Decision curve analysis of the net benefit of ExoGrail showed the potential to reduce the numbers of unnecessary biopsies by 35% when compared to current standards of care. Integration of information from multiple, non-invasive biomarker sources has the potential to greatly improve how patients with a clinical suspicion of prostate cancer are risk-assessed prior to an invasive biopsy.
A clinical oncolytic herpes simplex virus (HSV) encoding granulocyte-macrophage colony-stimulating factor (GM-CSF), talimogene laherparepvec, causes regression of injected and non-injected melanoma lesions in patients and is now licensed for clinical use in advanced melanoma. To date, limited data are available regarding the mechanisms of human anti-tumor immune priming, an improved understanding of which could inform the development of future combination strategies with improved efficacy. This study addressed direct oncolysis and innate and adaptive human immune-mediated effects of a closely related HSV encoding GM-CSF (HSVGM-CSF) alone and in combination with histone deacetylase inhibition. We found that HSVGM-CSF supported activation of anti-melanoma immunity via monocyte-mediated type I interferon production, which activates NK cells, and viral maturation of immature dendritic cells (iDCs) into potent antigen-presenting cells for cytotoxic T lymphocyte (CTL) priming. Addition of the histone deacetylase inhibitor valproic acid (VPA) to HSVGM-CSF treatment of tumor cells increased viral replication, viral GM-CSF production, and oncolysis and augmented the development of anti-tumor immunity. Mechanistically, VPA increased expression of activating ligands for NK cell recognition and induced expression of tumor-associated antigens, supporting innate NK cell killing and CTL priming. These data support the clinical combination of talimogene laherparepvec with histone deacetylase inhibition to enhance oncolysis and anti-tumor immunity.
Background: Sunitinib is a first line treatment for majority of patients with metastatic RCC. The recommended dose of 50mg often results in a spectrum of serious side effects which subsequently lead to dose reduction and may have an impact on response rates. Methods: We conducted a retrospective analysis of 62 RCC patients from single institution treated with sunitinib between September 2007-May 2010. Patients were stratified according to age groups, into ≤ 70 year old (y.o.) and > 70 y.o. to compare tolerability, response rates and median survival. Results: All patients were evaluable for toxicity, 55 patients were evaluable for response. 38 (61.2%) were ≤ 70 y.o. and 24 (38.8%) were >70y.o. 2 patients (5%) of ≤70 and 5 (20%) of > 70y.o. were non-evaluable for response due to early treatment discontinuation. The response rate was 36% in ≤70y.o. and 21% in >70 y.o., stable disease (SD) was observed in 41% ≤70 y.o. vs 47% in the older age group and progressive disease PD:22% vs 31.5% respectively. 24 (38.7%) of patients required dose reductions after the first or second cycle- 12 (33%) in ≤70 vs 11 (59%) in >70 yrs old. A small number of patients presented with PS 2 and these were started on a reduced dose of 37.5mg: 3 (8%) in ≤70y.o. and 11 (58%) > 70y.o. Toxcities were comparable in both groups however grade 3 palmar-plantar erythema (PPE) and mucositis (18% vs 1.6% and 18 vs 8% respectively) were more prevalent in the younger cohort. Grade 3 diarrhoea and fatigue were more common in older patients (10% in >70y.o vs 1.6% in ≤70y.o. and 16% vs 9.6% respectively). Median survival was 23 months for both age groups. Conclusions: Elderly patients more commonly require dose reduction due to poor performance status and toxicity profile. The objective response rate is lower with the lower dose intensity however the rate of disease stabilisation is comparable in both groups. The lower dose of Sunitinib is well tolerated in the elderly and this regimen should be considered for older patients with poor performance status.
In our clinical trials of oncolytic vesicular stomatitis virus expressing interferon beta (VSV-IFNβ), several patients achieved initial responses followed by aggressive relapse. We show here that VSV-IFNβ-escape tumors predictably express a point-mutated CSDE1 form of the RNA-binding Cold Shock Domain-containing E1 protein, which promotes escape as an inhibitor of VSV replication by disrupting viral transcription. Given time, VSV-IFNβ evolves a compensatory mutation in the P/M Inter-Genic Region which rescues replication in CSDE1 cells. These data show that CSDE1 is a major cellular co-factor for VSV replication. However, CSDE1 also generates a neo-epitope recognized by non-tolerized T cells. We exploit this predictable neo-antigenesis to drive, and trap, tumors into an escape phenotype, which can be ambushed by vaccination against CSDE1 , preventing tumor escape. Combining frontline therapy with escape-targeting immunotherapy will be applicable across multiple therapies which drive tumor mutation/evolution and simultaneously generate novel, targetable immunopeptidomes associated with acquired treatment resistance.
Prostate cancer is the most common malignant tumour in men. Improved testing for di- agnosis, risk prediction, and response to treatment would improve care. Here, we identified a pro- teomic signature of prostate cancer in peripheral blood using data-independent acquisition mass spectrometry combined with machine learning. A highly predictive signature was derived, which was associated with relevant pathways, including the coagulation, complement, and clotting cas- cades, as well as plasma lipoprotein particle remodeling. We further validated the identified bi- omarkers against a second cohort, identifying a panel of five key markers (GP5, SERPINA5, ECM1, IGHG1, and THBS1) which retained most of the diagnostic power of the overall dataset, achieving an AUC of 0.91. Taken together, this study provides a proteomic signature complementary to PSA for the diagnosis of patients with localised prostate cancer, with the further potential for assessing risk of future development of prostate cancer. Data are available via ProteomeXchange with identi- fier PXD025484.
Background: Prostate cancer (PCa) is the most common male cancer in the United Kingdom and we aimed to identify clinically relevant biomarkers corresponding to stage progression of the disease. Methods: We used enhanced proteomic profiling of PCa progression using iTRAQ 3D LC mass spectrometry on high-quality serum samples to identify biomarkers of PCa. Results: We identified >1000 proteins. Following specific inclusion/exclusion criteria we targeted seven proteins of which two were validated by ELISA and six potentially interacted forming an ‘interactome’ with only a single protein linking each marker. This network also includes accepted cancer markers, such as TNF, STAT3, NF-κB and IL6. Conclusions: Our linked and interrelated biomarker network highlights the potential utility of six of our seven markers as a panel for diagnosing PCa and, critically, in determining the stage of the disease. Our validation analysis of the MS-identified proteins found that SAA alongside KLK3 may improve categorisation of PCa than by KLK3 alone, and that TSR1, although not significant in this model, might also be a clinically relevant biomarker.
Lipids play a key role in many biological processes, and their accurate measurement is critical to unraveling the biology of diseases and human health. A high throughput HILIC-based (LC-MS) method for the semiquantitative screening of over 2000 lipids, based on over 4000 MRM transitions, was devised to produce an accessible and robust lipidomic screen for phospholipids in human plasma/serum. This methodology integrates many of the advantages of global lipid analysis with those of targeted approaches. Having used the method as an initial "wide class" screen, it can then be easily adapted for a more targeted analysis and quantification of key, dysregulated lipids. Robustness was assessed using 1550 continuous injections of plasma extracts onto a single column and via the evaluation of columns from 5 different batches of stationary phase. Initial screens in positive (239 lipids, 431 MRM transitions) and negative electrospray ionization (ESI) mode (232 lipids, 446 MRM transitions) were assessed for reproducibility, sensitivity, and dynamic range using analysis times of 8 min. The total number of lipids monitored using these screening methods was 433 with an overlap of 38 lipids in both modes. A polarity switching method for accurate quantification, using the same LC conditions, was assessed for intra- and interday reproducibility, accuracy, dynamic range, stability, carryover, dilution integrity, and matrix interferences and found to be acceptable. This polarity switching method was then applied to lipids important in the stratification of human prostate cancer samples.
Despite significant advances in our understanding of the molecular pathology of bladder cancer, it remains a significant health problem with high morbidity and mortality associated with muscle-invasive bladder cancer (stages T2+), and high costs associated with the surveillance of non-muscle-invasive bladder cancer (NMIBC, stages Ta/T1/Tis). Moreover, current diagnostic biomarkers are suboptimal and of poor utility for low grade disease and surveillance. In this study, we show that the Engrailed-2 (EN2) transcription factor is expressed in, and secreted by, bladder cancer cell lines and patient tumour specimens, justifying an evaluation of urinary EN2 as a diagnostic biomarker in bladder cancer using archived samples from an established biospecimen collection. In patients with NMIBC, urinary EN2 was detected in most cases with an overall sensitivity of 82% and specificity of 75%. The sensitivity for stage Ta and T1 tumours was 71% and 76%, respectively, and 94% for stage T2+ tumours. This compares favourably with existing markers. The sensitivity for tumour grades 1, 2 and 3 was 69%, 78% and 87%, respectively. Thus urinary EN2 has the potential to be a more sensitive and specific protein biomarker for NMIBC than currently available tests.
Genome-wide association studies (GWAS) have identified numerous common prostate cancer (PrCa) susceptibility loci. We have fine-mapped 64 GWAS regions known at the conclusion of the iCOGS study using large-scale genotyping and imputation in 25 723 PrCa cases and 26 274 controls of European ancestry. We detected evidence for multiple independent signals at 16 regions, 12 of which contained additional newly identified significant associations. A single signal comprising a spectrum of correlated variation was observed at 39 regions; 35 of which are now described by a novel more significantly associated lead SNP, while the originally reported variant remained as the lead SNP only in 4 regions. We also confirmed two association signals in Europeans that had been previously reported only in East-Asian GWAS. Based on statistical evidence and linkage disequilibrium (LD) structure, we have curated and narrowed down the list of the most likely candidate causal variants for each region. Functional annotation using data from ENCODE filtered for PrCa cell lines and eQTL analysis demonstrated significant enrichment for overlap with bio-features within this set. By incorporating the novel risk variants identified here alongside the refined data for existing association signals, we estimate that these loci now explain ∼38.9% of the familial relative risk of PrCa, an 8.9% improvement over the previously reported GWAS tag SNPs. This suggests that a significant fraction of the heritability of PrCa may have been hidden during the discovery phase of GWAS, in particular due to the presence of multiple independent signals within the same region
Coffee consumption has been shown in some studies to be associated with lower risk of prostate cancer. However, it is unclear if this association is causal or due to confounding or reverse causality. We conducted a Mendelian randomisation analysis to investigate the causal effects of coffee consumption on prostate cancer risk and progression. We used two genetic variants robustly associated with caffeine intake (rs4410790 and rs2472297) as proxies for coffee consumption in a sample of 46,687 men of European ancestry from 25 studies in the PRACTICAL consortium. Associations between genetic variants and prostate cancer case status, stage and grade were assessed by logistic regression and with all-cause and prostate cancer-specific mortality using Cox proportional hazards regression. There was no clear evidence that a genetic risk score combining rs4410790 and rs2472297 was associated with prostate cancer risk (OR per additional coffee increasing allele: 1.01, 95% CI: 0.98,1.03) or having high-grade compared to low-grade disease (OR: 1.01, 95% CI: 0.97,1.04). There was some evidence that the genetic risk score was associated with higher odds of having nonlocalised compared to localised stage disease (OR: 1.03, 95% CI: 1.01, 1.06). Amongst men with prostate cancer, there was no clear association between the genetic risk score and all-cause mortality (HR: 1.00, 95% CI: 0.97,1.04) or prostate cancer-specific mortality (HR: 1.03, 95% CI: 0.98,1.08). These results, which should have less bias from confounding than observational estimates, are not consistent with a substantial effect of coffee consumption on reducing prostate cancer incidence or progression.
Background Prevention of unnecessary biopsies and overtreatment of indolent disease remains a challenge in the management of prostate cancer. Novel non-invasive tests that can identify clinically significant (intermediate-risk and high-risk) diseases are needed to improve risk stratification and monitoring of prostate cancer patients. Here, we investigated a panel of six DNA methylation biomarkers in urine samples collected post-digital rectal exam from patients undergoing prostate biopsy, for their utility to guide decision making for diagnostic biopsy and early detection of aggressive prostate cancer. Results We recruited 408 patients in risk categories ranging from benign to low-, intermediate-, and high-risk prostate cancer from three international cohorts. Patients were separated into 2/3 training and 1/3 validation cohorts. Methylation biomarkers were analyzed in post-digital rectal exam urinary sediment DNA by quantitative MethyLight assay and investigated for their association with any or aggressive prostate cancers. We developed a Prostate Cancer Urinary Epigenetic (ProCUrE) assay based on an optimal two-gene (HOXD3 and GSTP1) LASSO model, derived from methylation values in the training cohort, and assessed ProCUrE’s diagnostic and prognostic ability for prostate cancer in both the training and validation cohorts. ProCUrE demonstrated improved prostate cancer diagnosis and identification of patients with clinically significant disease in both the training and validation cohorts. Using three different risk stratification criteria (Gleason score, D’Amico criteria, and CAPRA score), we found that the positive predictive value for ProCUrE was higher (59.4–78%) than prostate specific antigen (PSA) (38.2–72.1%) for all risk category comparisons. ProCUrE also demonstrated additive value to PSA in identifying GS ≥ 7 PCa compared to PSA alone (DeLong’s test p = 0.039), as well as additive value to the PCPT risk calculator for identifying any PCa and GS ≥ 7 PCa (DeLong’s test p = 0.011 and 0.022, respectively). Conclusions ProCUrE is a promising non-invasive urinary methylation assay for the early detection and prognostication of prostate cancer. ProCUrE has the potential to supplement PSA testing to identify patients with clinically significant prostate cancer.
PURPOSE: To conduct a phase I clinical trial with a second-generation oncolytic herpes simplex virus (HSV) expressing granulocyte macrophage colony-stimulating factor (Onco VEXGM-CSF) to determine the safety profile of the virus, look for evidence of biological activity, and identify a dosing schedule for later studies. EXPERIMENTAL DESIGN: The virus was administered by intratumoral injection in patients with cutaneous or s.c. deposits of breast, head and neck and gastrointestinal cancers, and malignant melanoma who had failed prior therapy. Thirteen patients were in a single-dose group, where doses of 10(6), 10(7), and 10(8) plaque-forming units (pfu)/mL were tested, and 17 patients were in a multidose group testing a number of dose regimens. RESULTS: The virus was generally well tolerated with local inflammation, erythema, and febrile responses being the main side effects. The local reaction to injection was dose limiting in HSV-seronegative patients at 10(7) pfu/mL. The multidosing phase thus tested seroconverting HSV-seronegative patients with 10(6) pfu/mL followed by multiple higher doses (up to 10(8) pfu/mL), which was well tolerated by all patients. Biological activity (virus replication, local reactions, granulocyte macrophage colony-stimulating factor expression, and HSV antigen-associated tumor necrosis), was observed. The duration of local reactions and virus replication suggested that dosing every 2 to 3 weeks was appropriate. Nineteen of 26 patient posttreatment biopsies contained residual tumor of which 14 showed tumor necrosis, which in some cases was extensive, or apoptosis. In all cases, areas of necrosis also strongly stained for HSV. The overall responses to treatment were that three patients had stable disease, six patients had tumors flattened (injected and/or uninjected lesions), and four patients showed inflammation of uninjected as well as the injected tumor, which, in nearly all cases, became inflamed. CONCLUSIONS: Onco VEXGM-CSF is well tolerated and can be safely administered using the multidosing protocol described. Evidence of an antitumor effect was seen.
Although genome-wide association studies have identified over 100 risk loci that explain ∼33% of familial risk for prostate cancer (PrCa), their functional effects on risk remain largely unknown. Here we use genotype data from 59,089 men of European and African American ancestries combined with cell-type-specific epigenetic data to build a genomic atlas of single-nucleotide polymorphism (SNP) heritability in PrCa. We find significant differences in heritability between variants in prostate-relevant epigenetic marks defined in normal versus tumour tissue as well as between tissue and cell lines. The majority of SNP heritability lies in regions marked by H3k27 acetylation in prostate adenoc7arcinoma cell line (LNCaP) or by DNaseI hypersensitive sites in cancer cell lines. We find a high degree of similarity between European and African American ancestries suggesting a similar genetic architecture from common variation underlying PrCa risk. Our findings showcase the power of integrating functional annotation with genetic data to understand the genetic basis of PrCa.
Recent advances in the treatment of metastatic renal cell carcinoma expose a gap in the treatment of less advanced, localized disease. Tyrosine kinase inhibitors, which revolutionized the treatment of metastatic disease, have not provided a similar survival benefit in the adjuvant setting and currently only sunitinib is approved by the Food and Drug Administration for adjuvant treatment in patients with high-risk of recurrence based on S-TRAC disease-free survival data. The advent of immune checkpoint inhibitors has offered a fresh hope in the field of adjuvant treatment after encouraging results are seen with combination of immune checkpoint inhibitors as well as with targeted therapy in the metastatic setting. Several studies are investigating these combinations in the adjuvant setting, and it is hoped that they will bring about a better outcome for a largely unmet need in kidney cancer treatment.
Melanoma is an aggressive skin cancer that carries an extremely poor prognosis when local invasion, nodal spread or systemic metastasis has occurred. Recent advances in melanoma biology have revealed that RAS-RAF-MEK-ERK signaling has a pivotal role in governing disease progression and treatment resistance. Proof-of-concept clinical studies have shown that direct BRAF inhibition yields impressive responses in advanced disease but these are short-lived as treatment resistance rapidly emerges. Therefore, there is a pressing need to develop new targeted strategies for BRAF mutant melanoma. As such, oncolytic viruses represent a promising cancer-specific approach with significant activity in melanoma. This study investigated interactions between genetically-modified vaccinia virus (GLV-1h68) and radiotherapy in melanoma cell lines with BRAF mutant, Ras mutant or wild-type genotype. Preclinical studies revealed that GLV-1h68 combined with radiotherapy significantly increased cytotoxicity and apoptosis relative to either single agent in V600D BRAF/V600E mutant melanoma in vitro and in vivo. The mechanism of enhanced cytotoxicity with GLV-1h68/radiation (RT) was independent of viral replication and due to attenuation of JNK, p38 and ERK MAPK phosphorylation specifically in BRAF mutant cells. Further studies showed that JNK pathway inhibition sensitized BRAF mutant cells to GLV-1h68-mediated cell death, mimicking the effect of RT. GLV-1h68 infection activated MAPK signaling in V600D BRAF/V600E BRAF mutant cell lines and this was associated with TNF-α secretion which, in turn, provided a prosurvival signal. Combination GLV-1h68/RT (or GLV-1h68/JNK inhibition) caused abrogation of TNF-α secretion. These data provide a strong rationale for combining GLV-1h68 with irradiation inV600D/E BRAF mutant tumors. © 2014 Macmillan Publishers Limited.
A DNA vaccine, SCIB1, incorporating two CD8 and two CD4 epitopes from TRP-2/gp100 was evaluated in patients with metastatic melanoma. Each patient received SCIB1 via intramuscular injection with electroporation. The trial was designed to find the safest dose of SCIB1 which induced immune/clinical responses in patients with or without tumour. Fifteen patients with tumor received SCIB1 doses of 0.4-8 mg whilst 20 fully-resected patients received 2–8 mg doses. Twelve patients elected to continue immunization every 3 months for up to 39 months. SCIB1 induced dose-dependent T cell responses in 88% of patients with no serious adverse effects or dose limiting toxicities. The intensity of the T cell responses was significantly higher in patients receiving 4 mg doses without tumor when compared to those with tumor (p ˂ 0.01). In contrast, patients with tumor showed a significantly higher response to the 8 mg dose than the 4 mg dose (p ˂ 0.03) but there was no significant difference in the patients without tumor. One of 15 patients with measurable disease showed an objective tumor response and 7/15 showed stable disease. 5/20 fully-resected patients have experienced disease recurrence but all remained alive at the cut-off date with a median observation time of 37 months. A positive clinical outcome was associated with MHC-I and MHC-II expression on tumors prior to therapy (p = 0.027). We conclude that SCIB1 is well tolerated and stimulates potent T cell responses in melanoma patients. It deserves further evaluation as a single agent adjuvant therapy or in combination with checkpoint inhibitors in advanced disease.
The HOX genes are a family of homeodomain-containing transcription factors that determine the identity of cells and tissues during embryonic development. They are also known to behave as oncogenes in some haematological malignancies. In this study we show that the expression of many of the HOX genes is highly elevated in primary non-small cell lung cancers and in the derived cell lines A549 and H23. Furthermore, blocking the activity of HOX proteins by interfering with their binding to the PBX co-factor causes these cells to undergo apoptosis in vitro and reduces the growth of A549 tumours in vivo. These findings suggest that the interaction between HOX and PBX proteins is a potential therapeutic target in non-small cell lung cancer.
Abstract Introduction: Triple Negative Breast Cancer (TNBC) is a heterogeneous disease, clinically defined for its aggressive tumour behaviour, metastatic ability and poor prognosis. Homeobox (HOX) genes are a family of homeodomain-containing transcription factors, which establish and maintain the identity and fate of cells and tissues during normal embryogenesis and organ development. A total of 39 HOX genes exist, located in four clusters (A-D) on different chromosomes. HOX genes are dysregulated in most cancers and they have an established role in driving key processes in breast carcinogenesis, including the regulation of the cell cycle, apoptosis, angiogenesis and metastasis. In this study, we evaluated the anti-tumour efficacy of a novel inhibitor of HOX protein function, HTL-001, which antagonizes the interactions between HOX proteins and their PBX cofactors. HTL-001, developed by HOX Therapeutics Ltd, is a synthetic peptide of 18 amino acids, comprised of a hexapeptide sequence, which resembles that on HOX proteins of paralogs 1-9, and a short C-terminal polyarginine sequence for cell penetration. We evaluated the efficacy of HTL-001 in vitro as a monotherapy in all cell lines representing all molecular classifications of breast cancer and in combination with chemotherapeutics for TNBC therapy. Most importantly, HTL-001 was examined in MDA-MB-231-BR cells, which have a propensity to metastasise to the brain, reflecting the disease course frequently observed in human patients. Methods: The differential expression of HOX and PBX genes in all subtypes of breast cancer was evaluated using bioinformatics analysis of TCGA and Oncomine data. The sensitivity to HTL-001 of breast cancer-derived cell lines of different molecular classifications, was determined using Cell Proliferation (MTS) Assay and FACS-based Annexin Assay. The anti-tumour effect of HTL-001 in combination with various chemotherapeutics was assessed and analysed for synergy using Bliss Analysis. The expression of genes previously shown to respond to HOX/PBX inhibition was measured from extracted RNA and protein using RT-qPCR and western blotting, respectively. The in vivo efficacy of HTL-001 will be investigated using a mouse flank tumour xenograft model with MDA-MB-231-BR cells, representative of TNBC. Results: TCGA and Oncomine data analysis showed TNBC tumours have a unique signature of HOX gene dysregulation, different to that of all other types of breast tumours, relative to normal breast tissues; most importantly upregulation in HOXB2 and HOXB3 genes. Targeting HOX/PBX dimers with HTL-001, induced apoptotic cell death in all breast cancer cell lines including; MCF-7, ZR-75-1, MDA-MB-231, BT-20 and SK-BR-3, with the highest sensitivity seen in brain seeking MDA-MB-231-BR cells. HTL-001 significantly upregulated the expression of key apoptotic and anti-survival genes including; AIF, cFOS, and DUSP1, resulting in the induction of apoptotic cell death in all breast cancer cell lines tested. Furthermore, we observed high levels of synergy between HTL-001 and the chemotherapeutic agents, Paclitaxel, Palbociclib and 5-Fluorouracil. Conclusion: HTL-001 is a novel inhibitor of HOX and PBX protein interactions capable of marked in vitro cytotoxicity in all types of breast cancer cells, particularly in TNBC. HTL-001 induced rapid apoptosis and triggered a downstream unique signature after target engagement. HTL-001 is currently the only therapy which targets HOX gene dysregulation and in doing so, may help address the current urgent unmet therapeutic need in TNBC through its unique mechanism of action and high levels of synergy with conventional anti-cancer agents. Citation Format: Einthavy Arunachalam, Guy R Simpson, Carla Sofia Möller-Levet, Nicola Annels, Richard Morgan, Timothy Robert Crook, Hardev Singh Pandha. Therapeutic targeting of HOX gene dysregulation in triple negative breast cancer [abstract]. In: Proceedings of the 2019 San Antonio Breast Cancer Symposium; 2019 Dec 10-14; San Antonio, TX. Philadelphia (PA): AACR; Cancer Res 2020;80(4 Suppl):Abstract nr P3-10-15.
Improving the chances of curing patients with cancer who have had surgery to remove metastatic sites of disease is a priority area for cancer research. Pexa-Vec (Pexastimogene Devacirepvec; JX-594, TG6006) is a principally immunotherapeutic oncolytic virus that has reached late-phase clinical trials. We report the results of a single-center, nonrandomized biological end point study (trial registration: EudraCT number 2012-000704-15), which builds on the success of the presurgical intravenous delivery of oncolytic viruses to tumors. Nine patients with either colorectal cancer liver metastases or metastatic melanoma were treated with a single intravenous infusion of Pexa-Vec ahead of planned surgical resection of the metastases. Grade 3 and 4 Pexa-Vec-associated side effects were lymphopaenia and neutropaenia. Pexa-Vec was peripherally carried in plasma and was not associated with peripheral blood mononuclear cells. Upon surgical resection, Pexa-Vec was found in the majority of analyzed tumors. Pexa-Vec therapy associated with IFNα secretion, chemokine induction, and resulted in transient innate and long-lived adaptive anticancer immunity. In the 2 patients with significant and complete tumor necrosis, a reduction in the peripheral T-cell receptor diversity was observed at the time of surgery. These results support the development of presurgical oncolytic vaccinia virus-based therapies to stimulate anticancer immunity and increase the chances to cure patients with cancer.
The apolipoprotein B mRNA editing enzyme catalytic polypeptide (APOBEC) family protects against infection by degrading incoming viral genomes through cytosine deamination. Here, we review how the potential to unleash these potent DNA mutagens comes at a price as APOBEC DNA mutagenesis can contribute to development of multiple types of cancer. In addition, because viral infection induces its expression, APOBEC is seen as the enemy of oncolytic virotherapy through mutation of the viral genome and by generating virotherapy-resistant tumors. Therefore, overall APOBEC in cancer has received very poor press. However, we also speculate how there may be silver linings to the storm douds (kataegis) associated with APOBEC activity. Thus, although mutagenic genomic chaos promotes emergence of ever more aggressive subclones, it also provides significant opportunity for cytotoxic and immune therapies. In particular, the superpower of cancer immunotherapy derives in part from mutation, wherein generation of tumor neoantigens-neoantigenesis-exposes tumor cells to functional T-cell repertoires, and susceptibility to immune checkpoint blockade. Moreover, APOBECs may be able to induce suprathreshold levels of cellular mutation leading to mitotic catastrophe and direct tumor cell killing. Finally, we discuss the possibility that linking predictable APOBEC-induced mutation with escape from specific frontline therapies could identify mutated molecules/pathways that can be targeted with small molecules and/or immunotherapies in a Trap and Ambush strategy. Together, these considerations lead to the counterintuitive hypothesis that, instead of attempting to expunge and excoriate APOBEC activity in cancer therapy, it might be exploited-and even, counterintuitively, encouraged.
Advanced renal-cell carcinoma is a very difficult tumour to treat, and response rates to biological therapies are less than 20%. The identification of various molecular and cellular markers has led to the development of novel therapies. Despite evaluation of their association with histological subtype, immune infiltration, molecular markers of cell proliferation, p53 mutation, and growth-factor-receptor expression, none of these markers has proved better predictive factors than tumour stage and histological grade. The identification of tumour-associated antigens and the specificity of cellular immune responses have led to the development of targeted immunotherapy with monoclonal antibodies, radioimmunotherapy, and T-cell therapies. In this review, we evaluate a range of markers associated with renal-cell carcinoma and new treatment approaches based on tumour-associated antigens and, in particular, T-cell epitopes.
Engrailed (En) is a member of the homeobox gene family, which encodes a homeodomain-containing transcription factor that is essential during early development. The only known site of normal adult Engrailed protein (EN) expression is in the nervous system, and it has been implicated in the development of both young-onset Parkinson's disease as well as autism. Over-expression of EN has been linked to tumour development in adults, particularly in breast, prostate, melanoma and ovarian cancers, and there is a growing interest in its role as a diagnostic and prognostic biomarker. It is hoped that further work may confirm associations between En expression and therapy-resistant, poor prognosis cancers, similar to that identified with other homeobox gene profiles.
Correction to: Nature Genetics https://doi.org/10.1038/s41588-020-00748-0, published online 4 January 2021. In the version of this article originally published, the names of the equally contributing authors and jointly supervising authors were switched. The correct affiliations are: “These authors contributed equally: David V. Conti, Burcu F. Darst. These authors jointly supervised this work: David V. Conti, Rosalind A. Eeles, Zsofia Kote-Jarai, Christopher A. Haiman.” The error has been corrected in the HTML and PDF versions of the article.
The HOX genes are a highly conserved family of homeodomain-containing transcription factors that specify cell identity in early development and, subsequently, in a number of adult processes including hematopoiesis. The dysregulation of HOX genes is associated with a number of malignancies including acute myeloid leukemia (AML) and acute lymphoid leukemia (ALL), where they have been shown to support the immortalization of leukemic cells both as chimeric partners in fusion genes and when overexpressed in their wild type form. This review covers our current understanding of the role of HOX genes in normal hematopoiesis, AML and ALL, with particular emphasis on the similarities and differences of HOX function in these contexts, their hematopoietic downstream genes targets and implications for therapy.Leukemia accepted article preview online, 5 December 2012; doi:10.1038/leu.2012.356.
BackgroundOncolytic virus V937 showed activity and safety with intratumoral administration. This phase 1 study evaluated intravenous V937±pembrolizumab in patients with advanced solid tumors.MethodsPatients had advanced non-small cell lung cancer (NSCLC), urothelial cancer, metastatic castration-resistant prostate cancer, or melanoma in part A (V937 monotherapy), and metastatic NSCLC or urothelial cancer in part B (V937+pembrolizumab). Prior immunotherapy was permitted >28 days before study treatment. Patients received intravenous V937 on days 1, 3, and 5 (also on day 8 in part B) of the first 21-day cycle and on day 1 of subsequent cycles for eight cycles. Three ascending dose-escalation cohorts were studied. Dose-escalation proceeded if no dose-limiting toxicities (DLTs) occurred in cycle 1 of the previous cohort. In part B, patients also received pembrolizumab 200 mg every 3 weeks from day 8 for 2 years; dose-expansion occurred at the highest-dose cohort. Serial biopsies were performed.ResultsNo DLTs occurred in parts A (n=18) or B (n=85). Grade 3–5 treatment-related adverse events (AEs) were not observed in part A and were experienced by 10 (12%) patients in part B. The most frequent treatment-related AEs (any grade) in part B were fatigue (36%), pruritus (18%), myalgia (14%), diarrhea (13%), pyrexia (13%), influenza-like illness (12%), and nausea (12%). At the highest tested dose, median intratumoral V937 concentrations were 117,631 copies/mL on day 8, cycle 1 in part A (n=6) and below the detection limit for most patients (86% (19/22)) on day 15, cycle 1 in part B. Objective response rates were 6% (part A), 9% in the NSCLC dose-expansion cohort (n=43), and 20% in the urothelial cancer dose-expansion cohort (n=35).ConclusionsIntravenous V937+pembrolizumab had a manageable safety profile. Although V937 was detected in tumor tissue, in NSCLC and urothelial cancer, efficacy was not greater than that observed in previous studies with pembrolizumab monotherapy.Trial registration numberNCT02043665.
© 2013 Springer-Verlag London. All rights are reserved.Prostate cancer can present at any stage of the disease and very frequently does not cause any symptoms at all. Most cancers arise in the periphery of the prostate gland and cause symptoms only when they have grown to compress the urethra or invade the sphincter [1]. In recent years, more and more of prostate cancer patients from the western hemisphere are diagnosed at an earlier stage due to rising prevalence of prostate-specific antigen (PSA) testing [2]. A study by Cooperberg et al. analyzed trends in clinical presentation in 2,078 men diagnosed between 1989 and 2001. The proportion of patients with low-risk tumor characteristics rose from 29.8 % in 1989-1992 to 45.3 % in 1999-2001 [3]. Studies based on the Department of Defense Center for Prostate Disease (CPDR) found downward migration at higher stage [3]. The percentage of patients presenting with locally advanced (T3 to T4) disease fell from 19.2 % in 1988 to 4.4 % in 1998; rates of metastatic disease at diagnosis likewise declined from 14.1 % in 1988 to 3.3 % in 1998.
Multiple intravenous injections of a cDNA library, derived from human melanoma cell lines and expressed using the highly immunogenic vector vesicular stomatitis virus (VSV), cured mice with established melanoma tumors. Successful tumor eradication was associated with the ability of mouse lymphoid cells to mount a tumor-specific CD4 + interleukin (IL)-17 recall response in vitro. We used this characteristic IL-17 response to screen the VSV-cDNA library and identified three different VSV-cDNA virus clones that, when used in combination but not alone, achieved the same efficacy against tumors as the complete parental virus library. VSV-expressed cDNA libraries can therefore be used to identify tumor rejection antigens that can cooperate to induce anti-tumor responses. This technology should be applicable to antigen discovery for other cancers, as well as for other diseases in which immune reactivity against more than one target antigen contributes to disease pathology. © 2012 Nature America, Inc. All rights reserved.
Context: About 50–70% of patients with non-muscle invasive bladder cancer (NMIBC) experience relapse of disease. Objective: To establish a panel of protein biomarkers incorporated in a multiplexed microarray (BCa chip) and a classifier for diagnosing recurrent NMIBC. Materials and methods: Urine samples from 45 patients were tested. Diagnostic performance was evaluated by receiver operating characteristic (ROC) analysis. Results: A multi biomarker panel (ECadh, IL8, MMP9, EN2, VEGF, past recurrences, BCG therapies and stage at diagnosis) was identified yielding an area under the curve of 0.96. Discussion and conclusion: This biomarker panel represents a potential diagnostic tool for noninvasive diagnosis of recurrent NMIBC.
Reovirus is a naturally occurring oncolytic virus that has shown preclinical efficacy in the treatment of a wide range of tumor types and has now reached phase III testing in clinical trials. The anti-cancer activity of reovirus has been attributed to both its direct oncolytic activity and the enhancement of anti-tumor immune responses. In this study, we have investigated the direct effect of reovirus on acute myeloid leukemia (AML) cells and its potential to enhance innate immune responses against AML, including the testing of primary samples from patients. Reovirus was found to replicate in and kill AML cell lines, and to reduce cell viability in primary AML samples. The pro-inflammatory cytokine interferon alpha (IFNα) and the chemokine (C-C motif) ligand 5 (known as RANTES [regulated upon activation, normal T-cell expressed, and secreted]) were also secreted from AML cells in response to virus treatment. In addition, reovirus-mediated activation of natural killer (NK) cells, within the context of peripheral blood mononuclear cells, stimulated their anti-leukemia response, with increased NK degranulation and IFNγ production and enhanced killing of AML targets. These data suggest that reovirus has the potential as both a direct cytotoxic and an immunotherapeutic agent for the treatment of AML.
Oncolytic viruses (OV) are promising treatments for cancer, with several currently undergoing testing in randomised clinical trials. Measles virus (MV) has not yet been tested in models of human melanoma. This study demonstrates the efficacy of MV against human melanoma. It is increasingly recognised that an essential component of therapy with OV is the recruitment of host antitumour immune responses, both innate and adaptive. MV-mediated melanoma cell death is an inflammatory process, causing the release of inflammatory cytokines including type-1 interferons and the potent danger signal HMGB1. Here, using human in vitro models, we demonstrate that MV enhances innate antitumour activity, and that MV-mediated melanoma cell death is capable of stimulating a melanoma-specific adaptive immune response.Gene Therapy advance online publication, 15 December 2011; doi:10.1038/gt.2011.205.
In 2010, the US FDA approved the first therapeutic cancer vaccine for the treatment of castration refractory prostate cancer - sipuleucel-T. Prostate cancer is an ideal model for cancer vaccine development based on the ready demonstration of humoral and cellular immunity to a range of cancer antigens as well as often slow progression which means that patients who are otherwise well may have a radiologically evaluable minor progression, after conventional treatment and can undergo vaccine therapy over sufficient periods of time, so as to allow the generation of a robust antitumor response. The association of prostate cancer with one of the few serum cancer biomarkers in general use has also allowed assessment of response and risk stratification of patients. In this review, we will examine key aspects of the evolution of prostate cancer vaccines, which provides an accurate prototype for other cancers, and the challenges we face.
BACKGROUND: Approximately 4-25% of patients with early prostate cancer develop disease recurrence following radical prostatectomy. OBJECTIVE: To identify a molecular subgroup of prostate cancers with metastatic potential at presentation resulting in a high risk of recurrence following radical prostatectomy. DESIGN, SETTING & PARTICIPANTS: Unsupervised hierarchical clustering was performed using gene expression data from 70 primary resections, 31 metastatic lymph nodes and 25 normal prostate samples. Independent assay validation was performed using 322 radical prostatectomy samples from four sites with a mean follow-up of 50.3 months. OUTCOME MEASURES & STATISTICAL ANALYSIS: Molecular subgroups were identified using unsupervised hierarchical clustering. A partial least squares approach was used to generate a gene expression assay. Relationships with outcome (time to biochemical and metastatic recurrence) were analyzed using multivariable Cox regression and log-rank analysis. RESULTS & LIMITATIONS: A molecular subgroup of primary prostate cancer with biology similar to metastatic disease was identified. A 70-transcript signature (Metastatic Assay) was developed and independently validated in the radical prostatectomy samples. Metastatic Assay positive patients had increased risk of biochemical recurrence (Multivariable HR 1.62 [1.13-2.33]; p= 0.0092) and metastatic recurrence (Multivariable HR=3.20 (1.76-5.80); p=0.0001). A combined model with CAPRA-S identified patients at increased risk of biochemical and metastatic recurrence superior to either model alone (HR=2.67 [1.90-3.75]; p
Urothelial carcinoma of the urinary bladder (UCB) or bladder cancer remains a major health problem with high morbidity and mortality rates, especially in the western world. UCB is also associated with the highest cost per patient. In recent years numerous markers have been evaluated for suitability in UCB detection and surveillance. However, to date none of these markers can replace or even reduce the use of routine tools (cytology and cystoscopy). Our current study described UCB's extensive expression profile and highlighted the variations with normal bladder tissue. Our data revealed that JUP, PTGDR, KLRF1, MT-TC , and RNU6-135P are associated with prognosis in patients with UCB. The microarray expression data identified also S100A12, S100A8 , and NAMPT as potential UCB biomarkers. Pathway analysis revealed that natural killer cell mediated cytotoxicity is the most involved pathway. Our analysis showed that S100A12 protein may be useful as a biomarker for early UCB detection. Plasma S100A12 has been observed in patients with UCB with an overall sensitivity of 90.5% and a specificity of 75%. S100A12 is highly expressed preferably in high-grade and high-stage UCB. Furthermore, using a panel of more than hundred urine samples, a prototype lateral flow test for the transcription factor Engrailed-2 (EN2) also showed reasonable sensitivity (85%) and specificity (71%). Such findings provide confidence to further improve and refine the EN2 rapid test for use in clinical practice. In conclusion, S100A12 and EN2 have shown potential value as biomarker candidates for UCB patients. These results can speed up the discovery of biomarkers, improving diagnostic accuracy and may help the management of UCB.
BACKGROUND: Germline mutations within DNA-repair genes are implicated in susceptibility to multiple forms of cancer. For prostate cancer (PrCa), rare mutations in BRCA2 and BRCA1 give rise to moderately elevated risk, whereas two of ∼100 common, low-penetrance PrCa susceptibility variants identified so far by genome-wide association studies implicate RAD51B and RAD23B. METHODS: Genotype data from the iCOGS array were imputed to the 1000 genomes phase 3 reference panel for 21 780 PrCa cases and 21 727 controls from the Prostate Cancer Association Group to Investigate Cancer Associated Alterations in the Genome (PRACTICAL) consortium. We subsequently performed single variant, gene and pathway-level analyses using 81 303 SNPs within 20 Kb of a panel of 179 DNA-repair genes. RESULTS: Single SNP analyses identified only the previously reported association with RAD51B. Gene-level analyses using the SKAT-C test from the SNP-set (Sequence) Kernel Association Test (SKAT) identified a significant association with PrCa for MSH5. Pathway-level analyses suggested a possible role for the translesion synthesis pathway in PrCa risk and Homologous recombination/Fanconi Anaemia pathway for PrCa aggressiveness, even though after adjustment for multiple testing these did not remain significant. CONCLUSIONS: MSH5 is a novel candidate gene warranting additional follow-up as a prospective PrCa-risk locus. MSH5 has previously been reported as a pleiotropic susceptibility locus for lung, colorectal and serous ovarian cancers.
Purpose: Adjuvant sunitinib therapy compared with placebo prolonged disease-free survival (DFS) in patients with locoregional high-risk renal cell carcinoma in the S-TRAC trial (ClinicalTrials.gov number, NCT00375674). A prospectively-designed exploratory analysis of tissue biomarkers was conducted to identify predictors of treatment benefit. Experimental Design: Tissue blocks were used for immunohistochemistry (IHC) staining of PD-L1, CD4, CD8, and CD68. DFS was compared between < versus ≥ median IHC parameter using the Kaplan–Meier method. For biomarkers with predictive potential, Receiver Operating Characteristics curves were generated. Results: Baseline characteristics were similar in patients with (n=191) and without (n=419) IHC analysis. Among patients with IHC, longer DFS was observed in patients with tumor CD8+ T-cell density ≥ versus < median (median [95% CI], not reached [6.83–not reached] vs. 3.47 years [1.73–not reached]; hazard ratio 0.40 [95% CI, 0.20–0.81]; P=0.009) treated with sunitinib (n=101), but not with placebo (n=90). The sensitivity and specificity for CD8+ T-cell density in predicting DFS were 0.604 and 0.658, respectively. Shorter DFS was observed in placebo-treated patients with PD-L1+ versus PD-L1– tumors (hazard ratio 1.75; P=0.103). Among all patients with PD-L1+ tumors, DFS was numerically longer with sunitinib versus placebo (hazard ratio 0.58; P=0.175). Conclusions: Greater CD8+ T-cell density in tumor tissue was associated with longer DFS with sunitinib but not placebo, suggesting predictive treatment effect utility. Further independent cohort validation studies are warranted. The prognostic value of PD-L1 expression in primary tumors from patients with high-risk non-metastatic renal cell carcinoma should also be further explored.
The HOX genes are a family of closely related transcription factors that help to define the identity of cells and tissues during embryonic development and which are also frequently deregulated in a number of malignancies, including breast cancer. While relatively little is known about the roles that individual HOX genes play in cancer, it is however clear that these roles can be both contradictory, with some members acting as oncogenes and some as tumor suppressors, and also redundant, with several genes essentially having the same function. Here, we have attempted to address this complexity using the HXR9 peptide to target the interaction between HOX proteins and PBX, a second transcription factor that serves as a common co-factor for many HOX proteins. We show that HXR9 causes apoptosis in a number of breast cancer-derived cell lines and that sensitivity to HXR9 is directly related to the averaged expression of HOX genes HOXB1 through to HOXB9, providing a potential biomarker to predict the sensitivity of breast tumors to HXR9 or its derivatives. Measuring the expression of HOX genes HOXB1-HOXB9 in primary tumors revealed that a subset of tumors show highly elevated expression indicating that these might be potentially very sensitive to killing by HXR9. Furthermore, we show that while HXR9 blocks the oncogenic activity of HOX genes, it does not affect the known tumor-suppressor properties of a subset of HOX genes in breast cancer.
BACKGROUND: Epithelial ovarian cancer is a common malignancy, with no clinically approved diagnostic biomarker. Engrailed-2 (EN2) is a homeodomain-containing transcription factor, essential during embryological neural development, which is dysregulated in several cancer types. We evaluated the expression of EN2 in Epithelial ovarian cancer, and reviewed its role as a biomarker. METHODS We evaluated 8 Epithelial ovarian cancer cell lines, along with >100 surgical specimens from the Royal Surrey County Hospital (2009-2014). In total, 108 tumours and 5 normal tissue specimens were collected. En2 mRNA was evaluated by semi-quantitative RT-PCR. Histological sub-type, and platinum-sensitive/-resistant status were compared. Protein expression was assessed in cell lines (immunofluorescence), and in >150 tumours (immunohistochemistry). RESULTS En2 mRNA expression was elevated in serous ovarian tumours compared with normal ovary (p
Understanding how incompletely cleared primary tumors transition from minimal residual disease (MRD) into treatment resistant, immune-invisible recurrences has major clinical significance. We show here that this transition is mediated through the subversion of two key elements of innate immune surveillance. In the first, the role of TNFalpha changes from an antitumor effector against primary tumors into a growth promoter for MRD. Second, whereas primary tumors induced a natural killer (NK)-mediated cytokine response characterized by low IL6 and elevated IFNgamma, PD-L1hi MRD cells promoted the secretion of IL6 but minimal IFNgamma, inhibiting both NK cell and T-cell surveillance. Tumor recurrence was promoted by trauma- or infection-like stimuli inducing VEGF and TNFalpha which stimulated the growth of MRD tumors. Finally, therapies which blocked PD1, TNFalpha or NK cells delayed or prevented recurrence. These data show how innate immune surveillance mechanisms, which control infection and growth of primary tumors, are exploited by recurrent, competent tumors and identifies therapeutic targets in patients with MRD known to be at high risk of relapse.
Background: Evidence on height and prostate cancer risk is mixed, however, recent studies with large data sets support a possible role for its association with the risk of aggressive prostate cancer. Methods: We analysed data from the PRACTICAL consortium consisting of 6207 prostate cancer cases and 6016 controls and a subset of high grade cases (2480 cases). We explored height, polymorphisms in genes related to growth processes as main effects and their possible interactions. Results: The results suggest that height is associated with high-grade prostate cancer risk. Men with height 4180cm are at a 22% increased risk as compared to men with height o173cm (OR 1.22, 95% CI 1.01–1.48). Genetic variants in the growth pathway gene showed an association with prostate cancer risk. The aggregate scores of the selected variants identified a significantly increased risk of overall prostate cancer and high-grade prostate cancer by 13% and 15%, respectively, in the highest score group as compared to lowest score group. Conclusions: There was no evidence of gene-environment interaction between height and the selected candidate SNPs. Our findings suggest a role of height in high-grade prostate cancer. The effect of genetic variants in the genes related to growth is seen in all cases and high-grade prostate cancer. There is no interaction between these two exposures.
Breast, ovarian, and prostate cancers are hormone-related and may have a shared genetic basis but this has not been investigated systematically by genome-wide association (GWA) studies. Meta-analyses combining the largest GWA meta-analysis data sets for these cancers totaling 112,349 cases and 116,421 controls of European ancestry, all together and in pairs, identified at P < 10-8 seven new cross-cancer loci: three associated with susceptibility to all three cancers (rs17041869/2q13/BCL2L11; rs7937840/11q12/INCENP; rs1469713/19p13/GATAD2A), two breast and ovarian cancer risk loci (rs200182588/9q31/SMC2; rs8037137/15q26/RCCD1), and two breast and prostate cancer risk loci (rs5013329/1p34/NSUN4; rs9375701/6q23/L3MBTL3). Index variants in five additional regions previously associated with only one cancer also showed clear association with a second cancer type. Cell-type specific expression quantitative trait locus and enhancer-gene interaction annotations suggested target genes with potential cross-cancer roles at the new loci. Pathway analysis revealed significant enrichment of death receptor signaling genes near loci with P < 10-5 in the three-cancer meta-analysis.
There is an unmet need for improved diagnostic testing and risk prediction for cases of prostate cancer (PCa) to improve care and reduce overtreatment of indolent disease. Here we have analysed the serum proteome and lipidome of 262 study participants by liquid chromatography-mass spectrometry, including participants diagnosed with PCa, benign prostatic hyperplasia (BPH), or otherwise healthy volunteers, with the aim of improving biomarker specificity. Although a two class machine learning model separated PCa from controls with sensitivity of 0.82 and specificity of 0.95, adding BPH resulted in a statistically significant decline in specificity for prostate cancer to 0.76, with half of BPH cases being misclassified by the model as PCa. A small number of biomarkers differentiating between BPH and prostate cancer were identified, including proteins in MAP Kinase pathways, as well as in lipids containing oleic acid; these may offer a route to greater specificity. These results highlight, however, that whilst there are opportunities for machine learning, these will only be achieved by use of appropriate training sets that include confounding comorbidities, especially when calculating the specificity of a test.
As a clinical setting in which local live biological therapy is already well established, non-muscle invasive bladder cancer (NMIBC) presents intriguing opportunities for oncolytic virotherapy. Coxsackievirus A21 (CVA21) is a novel intercellular adhesion molecule-1 (ICAM-1)-targeted immunotherapeutic virus. This study investigated CVA21-induced cytotoxicity in a panel of human bladder cancer cell lines, revealing a range of sensitivities largely correlating with expression of the viral receptor ICAM-1. CVA21 in combination with low doses of mitomycin-C enhanced CVA21 viral replication and oncolysis by increasing surface expression levels of ICAM-1. This was further confirmed using 300-μm precision slices of NMIBC where levels of virus protein expression and induction of apoptosis were enhanced with prior exposure to mitomycin-C. Given the importance of the immunogenicity of dying cancer cells for triggering tumor-specific responses and long-term therapeutic success, the ability of CVA21 to induce immunogenic cell death was investigated. CVA21 induced immunogenic apoptosis in bladder cancer cell lines, as evidenced by expression of the immunogenic cell death (ICD) determinant calreticulin, and HMGB-1 release and the ability to reject MB49 tumors in syngeneic mice after vaccination with MB49 cells undergoing CVA21 induced ICD. Such CVA21 immunotherapy could offer a potentially less toxic, more effective option for the treatment of bladder cancer.
Background The oncolytic virus, coxsackievirus A21 (CVA21), has shown promise as a single agent in several clinical trials and is now being tested in combination with immune checkpoint blockade. Combination therapies offer the best chance of disease control; however, the design of successful combination strategies requires a deeper understanding of the mechanisms underpinning CVA21 efficacy, in particular, the role of CVA21 anti-tumor immunity. Therefore, this study aimed to examine the ability of CVA21 to induce human anti-tumor immunity, and identify the cellular mechanism responsible. Methods This study utilized peripheral blood mononuclear cells from i) healthy donors, ii) Acute Myeloid Leukemia (AML) patients, and iii) patients taking part in the STORM clinical trial, who received intravenous CVA21; patients receiving intravenous CVA21 were consented separately in accordance with local institutional ethics review and approval. Collectively, these blood samples were used to characterize the development of innate and adaptive anti-tumor immune responses following CVA21 treatment. Results An Initial characterization of peripheral blood mononuclear cells, collected from cancer patients following intravenous infusion of CVA21, confirmed that CVA21 activated immune effector cells in patients. Next, using hematological disease models which were sensitive (Multiple Myeloma; MM) or resistant (AML) to CVA21-direct oncolysis, we demonstrated that CVA21 stimulated potent anti-tumor immune responses, including: 1) cytokine-mediated bystander killing; 2) enhanced natural killer cell-mediated cellular cytotoxicity; and 3) priming of tumor-specific cytotoxic T lymphocytes, with specificity towards known tumor-associated antigens. Importantly, immune-mediated killing of both MM and AML, despite AML cells being resistant to CVA21-direct oncolysis, was observed. Upon further examination of the cellular mechanisms responsible for CVA21-induced anti-tumor immunity we have identified the importance of type I IFN for NK cell activation, and demonstrated that both ICAM-1 and plasmacytoid dendritic cells were key mediators of this response. Conclusion This work supports the development of CVA21 as an immunotherapeutic agent for the treatment of both AML and MM. Additionally, the data presented provides an important insight into the mechanisms of CVA21-mediated immunotherapy to aid the development of clinical biomarkers to predict response and rationalize future drug combinations.
Reovirus type 3 Dearing (T3D) has demonstrated oncolytic activity in vitro, in in vivo murine models and in early clinical trials. However the true potential of oncolytic viruses may only be realized fully in combination with other modalities such as chemotherapy, targeted therapy and radiotherapy. In this study, we examine the oncolytic activity of reovirus T3D and chemotherapeutic agents against human prostate cancer cell lines, with particular focus on the highly metastatic cell line PC3 and the chemotherapeutic agent docetaxel. Docetaxel is the standard of care for metastatic prostate cancer and acts by disrupting the normal process of microtubule assembly and disassembly. Reoviruses have been shown to associate with microtubules and may require this association for efficient viral replication.
The transferability and clinical value of genetic risk scores (GRSs) across populations remain limited due to an imbalance in genetic studies across ancestrally diverse populations. Here we conducted a multi-ancestry genome-wide association study of 156,319 prostate cancer cases and 788,443 controls of European, African, Asian and Hispanic men, reflecting a 57% increase in the number of non-European cases over previous prostate cancer genome-wide association studies. We identified 187 novel risk variants for prostate cancer, increasing the total number of risk variants to 451. An externally replicated multi-ancestry GRS was associated with risk that ranged from 1.8 (per standard deviation) in African ancestry men to 2.2 in European ancestry men. The GRS was associated with a greater risk of aggressive versus non-aggressive disease in men of African ancestry (P = 0.03). Our study presents novel prostate cancer susceptibility loci and a GRS with effective risk stratification across ancestry groups.
Oncolytic viruses are multifunctional anticancer agents with huge clinical potential, and have recently passed the randomized Phase III clinical trial hurdle. Both wild-type and engineered viruses have been selected for targeting of specific cancers, to elicit cytotoxicity, and also to generate antitumor immunity. Single-agent oncolytic virotherapy treatments have resulted in modest effects in the clinic. There is increasing interest in their combination with cytotoxic agents, radiotherapy and immune-checkpoint inhibitors. Similarly to oncolytic viruses, the benefits of chemotherapeutic agents may be that they induce systemic antitumor immunity through the induction of immunogenic cell death of cancer cells. Combining these two treatment modalities has to date resulted in significant potential in vitro and in vivo synergies through various mechanisms without any apparent additional toxicities. Chemotherapy has been and will continue to be integral to the management of advanced cancers. This review therefore focuses on the potential for a number of common cytotoxic agents to be combined with clinically relevant oncolytic viruses. In many cases, this combined approach has already advanced to the clinical trial arena. Keywords: oncolytic virotherapy, chemotherapy, immunogenic cell death
Extensive efforts to identify a clinically useful biomarker for the diagnosis of prostate cancer have resulted in important insights into the biology of the disease, but no new test has been approved by regulatory authorities. The unmet need has also shifted to identifying biomarkers that not only diagnose prostate cancer but also indicate whether the patient has 'significant' disease. EN2 is a homeobox-containing transcription factor secreted specifically by prostate cancers into urine, where it can be detected by a simple ELISA assay. A number of studies have demonstrated the enormous potential of EN2 to address this unmet need and provide the urologist with a simple, cheap and efficient prostate cancer biomarker.
Genome-wide association studies (GWAS) and fine-mapping efforts to date have identified more than 100 prostate cancer (PrCa)-susceptibility loci. We meta-analyzed genotype data from a custom high-density array of 46,939 PrCa cases and 27,910 controls of European ancestry with previously genotyped data of 32,255 PrCa cases and 33,202 controls of European ancestry. Our analysis identified 62 novel loci associated (P ˂ 5.0 × 10−8) with PrCa and one locus significantly associated with early-onset PrCa (≤55 years). Our findings include missense variants rs1800057 (odds ratio (OR) = 1.16; P = 8.2 × 10−9; G˃C, p.Pro1054Arg) in ATM and rs2066827 (OR = 1.06; P = 2.3 × 10−9; T˃G, p.Val109Gly) in CDKN1B. The combination of all loci captured 28.4% of the PrCa familial relative risk, and a polygenic risk score conferred an elevated PrCa risk for men in the ninetieth to ninety-ninth percentiles (relative risk = 2.69; 95% confidence interval (CI): 2.55–2.82) and first percentile (relative risk = 5.71; 95% CI: 5.04–6.48) risk stratum compared with the population average. These findings improve risk prediction, enhance fine-mapping, and provide insight into the underlying biology of PrCa.
Prostate cancer is the most common cancer in men in developed countries, and is a target for risk reduction strategies. The effects of alcohol consumption on prostate cancer incidence and survival remain unclear, potentially due to methodological limitations of observational studies. In the current study we investigated the associations of genetic variants in alcohol-metabolising genes with prostate cancer incidence and survival.
Background: Ovarian cancer remains the most lethal gynaecologic tumour in the Western world. Stimulation of the immune system to consolidate response to chemotherapy can potentially be beneficial however so far none of the vaccination strategies have offered survival advantage. Thus identifying and targeting clinically relevant antigens for immunotherapy continues to be an important research strategy. We have evaluated Engrailed-2 (EN2) as a potential target for vaccine strategy. EN2 is a homeodomain-containing transcription factor with a multifunctional role in neural development. There is evidence that over-expression of EN2 protein maybe linked to tumour development. Methods: Ovarian cancer cell lines were analysed by FACS for EN2 cell surface expression. EN2 expression in ovarian cancer tissue arrays were done by immunohistochemistry. A serum analysis (ELISA) was done to evaluate the presence of antibodies to EN2 in ovarian cancer patients and age-matched controls. A set of potentially immunogenic HLA-A2 restricted epitopes from the EN2 protein was identified using a computer algorithm SYFPEITHI. These peptides have been tested on HLA-A2 positive ovarian cancer patients’ PBMC using an in vitro culture method. The specificity of these T cell lines was analysed against T2 target cells loaded with or without EN2 peptides Results: Cell surface expression of EN2 was observed in ovarian cancer cell lines OVCAR3, OV90, CaOV-3, ES-2 and SKOV-3 of which ES-2 and SKOV3 showed strong expression. EN2 was also present in approximately 80% of ovarian cancer tissues whereas EN-2 expression was very low (
Renal cell carcinoma is an immunogenic tumour with a prominent dysfunctional immune cell infiltrate, unable to control tumour growth. Although tyrosine kinase inhibitors and immunotherapy have improved the outlook for some patients, many individuals are non-responders or relapse despite treatment. The hostile metabolic environment in RCC affects the ability of T-cells to maintain their own metabolic programme constraining T-cell immunity in RCC. We investigated the phenotype, function and metabolic capability of RCC TILs correlating this with clinicopathological features of the tumour and metabolic environment at the different disease stages. Flow cytometric analysis of freshly isolated TILs showed the emergence of exhausted T-cells in advanced disease based on their PD-1high and CD39 expression and reduced production of inflammatory cytokines upon in vitro stimulation. Exhausted T-cells from advanced stage disease also displayed an overall phenotype of metabolic insufficiency, characterized by mitochondrial alterations and defects in glucose uptake. Nanostring nCounter cancer metabolism assay on RNA obtained from 30 ccRCC cases revealed significant over-expression of metabolic genes even at early stage disease (pT1-2), while at pT3-4 and the locally advanced thrombi stages, there was an overall decrease in differentially expressed metabolic genes. Notably, the gene PPARGC1A was the most significantly down-regulated gene from pT1-2 to pT3-4 RCC which correlated with loss of mitochondrial function in tumour-infiltrating T-cells evident at this tumour stage. Down-regulation of PPARGC1A into stage pT3-4 may be the 'tipping-point' in RCC disease progression, modulating immune activity in ccRCC and potentially reducing the efficacy of immunotherapies in RCC and poorer patient outcomes.
The Open University's first one-day symposium on treatment-emergent neuroendocrine prostate cancer attracted world-leading figures, early career researchers and industry colleagues. The symposium proved insightful into the 'real-world' impact and current problems faced in the diagnosis and treatment of neuroendocrine prostate cancer. It was important for this meeting to take place as the incidence of neuroendocrine prostate cancer is increasing due to the widespread use of next-generation androgen deprivation drugs. The symposium discussions proposed new molecularly driven deadlines to accelerate research and improved the treatment of this deadly and poorly recognized malignancy.
PBX3 is a homeodomain-containing transcription factor of the pre-B cell leukemia (PBX) family, members of which have extensive roles in early development and some adult processes. A number of features distinguish PBX3 from other PBX proteins, including the ability to form specific and stable interactions with DNA in the absence of cofactors. PBX3 has frequently been reported as having a role in the development and maintenance of a malignant phenotype, and high levels of PBX3 tumor expression have been linked to shorter overall survival in cancer. In this review we consider the similarities and differences in the function of PBX3 in different cancer types and draw together the core signaling pathways involved to help provide a better insight into its potential as a therapeutic target.
There has been interest in using viruses to treat cancer for over a century. Recent clinical efforts, driven on by significant preclinical advances, have focussed on the safety of using replication-competent viruses. Recently published clinical trials of six oncolytic viruses (adenovirus, reovirus, measles, herpes simplex, Newcastle disease virus and vaccinia) have added to the accumulating data that endorse oncolytic viruses as a safe and well tolerated treatment approach. Conclusive evidence of efficacy remains to be demonstrated, but randomised clinical trials are now underway.
OBJECTIVE: Oncolytic forms of attenuated Vaccinia virus are now in clinical development, assessing the compatibility of this novel treatment with radiotherapy may reveal exploitable synergistic relationships. MATERIALS AND METHODS: In vitro analyses of cell killing, cell cycle effects and caspase activation were carried out on HN3, HN5, CAL27, Detroit, SIHN5B, and PJ41 cells. In vivo studies of the virus and X-radiation were performed on H&N xenografts in CD1 nude mice. RESULTS: Cell killing in vitro was demonstrated to be dose- and time-dependent. Infection causes an increase in S-phase and sub-G1 cells. A dose dependent increase in active caspase-3 indicated induction of apoptosis. Xenografts injected with Vaccinia stabilised and frequently completely regressed. Combination with radiation generated additional cell death, induction of caspase activity and in vivo further improved long term regression rates. CONCLUSIONS: These data support continued exploration of this therapy combination and indicates potential for clinical trials in head and neck cancer.
The HOX genes are a family of homeodomain-containing transcription factors that determine cellular identity during development. Here we review a number of recent studies showing that HOX genes are strongly expressed in ovarian cancer, and that in some cases the expression of specific HOX genes is sufficient to confer a particular identity and phenotype upon cancer cells. We also review the recent advances in elucidating the different functions of HOX genes in ovarian cancer. A literature search was performed using the search terms HOX genes (including specific HOX genes), ovarian cancer and oncogenesis. Articles were accessed through searches performed in ISI Web of Knowledge, PubMed and ScienceDirect. Taken together, these studies have shown that HOX genes play a role in the oncogenesis of ovarian cancer and function in the inhibition of apoptosis, DNA repair and enhanced cell motility. The function of HOX genes in ovarian cancer oncogenesis supports their potential role as prognostic and diagnostic markers, and as therapeutic targets in this disease.
Oncolytic viruses, which preferentially lyse cancer cells and stimulate an antitumor immune response, represent a promising approach to the treatment of cancer. However, how they evade the antiviral immune response and their selective delivery to, and replication in, tumor over normal tissue has not been investigated in humans. Here, we treated patients with a single cycle of intravenous reovirus before planned surgery to resect colorectal cancer metastases in the liver. Tracking the viral genome in the circulation showed that reovirus could be detected in plasma and blood mononuclear, granulocyte, and platelet cell compartments after infusion. Despite the presence of neutralizing antibodies before viral infusion in all patients, replication-competent reovirus that retained cytotoxicity was recovered from blood cells but not plasma, suggesting that transport by cells could protect virus for potential delivery to tumors. Analysis of surgical specimens demonstrated greater, preferential expression of reovirus protein in malignant cells compared to either tumor stroma or surrounding normal liver tissue. There was evidence of viral factories within tumor, and recovery of replicating virus from tumor (but not normal liver) was achieved in all four patients from whom fresh tissue was available. Hence, reovirus could be protected from neutralizing antibodies after systemic administration by immune cell carriage, which delivered reovirus to tumor. These findings suggest new preclinical and clinical scheduling and treatment combination strategies to enhance in vivo immune evasion and effective intravenous delivery of oncolytic viruses to patients in vivo.
BACKGROUND Sunitinib, a vascular endothelial growth factor pathway inhibitor, is an effective treatment for metastatic renal-cell carcinoma. We sought to determine the efficacy and safety of sunitinib in patients with locoregional renal-cell carcinoma at high risk for tumor recurrence after nephrectomy. METHODS In this randomized, double-blind, phase 3 trial, we assigned 615 patients with locoregional, high-risk clear-cell renal-cell carcinoma to receive either sunitinib (50 mg per day) or placebo on a 4-weeks-on, 2-weeks-off schedule for 1 year or until disease recurrence, unacceptable toxicity, or consent withdrawal. The primary end point was disease-free survival, according to blinded independent central review. Secondary end points included investigator-assessed disease-free survival, overall survival, and safety. RESULTS The median duration of disease-free survival was 6.8 years (95% confidence interval [CI], 5.8 to not reached) in the sunitinib group and 5.6 years (95% CI, 3.8 to 6.6) in the placebo group (hazard ratio, 0.76; 95% CI, 0.59 to 0.98; P=0.03). Overall survival data were not mature at the time of data cutoff. Dose reductions because of adverse events were more frequent in the sunitinib group than in the placebo group (34.3% vs. 2%), as were dose interruptions (46.4% vs. 13.2%) and discontinuations (28.1% vs. 5.6%). Grade 3 or 4 adverse events were more frequent in the sunitinib group (48.4% for grade 3 events and 12.1% for grade 4 events) than in the placebo group (15.8% and 3.6%, respectively). There was a similar incidence of serious adverse events in the two groups (21.9% for sunitinib vs. 17.1% for placebo); no deaths were attributed to toxic effects. CONCLUSIONS Among patients with locoregional clear-cell renal-cell carcinoma at high risk for tumor recurrence after nephrectomy, the median duration of disease-free survival was significantly longer in the sunitinib group than in the placebo group, at a cost of a higher rate of toxic events. (Funded by Pfizer; S-TRAC ClinicalTrials.gov number, NCT00375674.)
Objectives To develop a risk classifier using urine‐derived extracellular vesicle (EV)‐RNA capable of providing diagnostic information on disease status prior to biopsy, and prognostic information for men on active surveillance (AS). Patients and Methods Post‐digital rectal examination urine‐derived EV‐RNA expression profiles (n = 535, multiple centres) were interrogated with a curated NanoString panel. A LASSO‐based continuation ratio model was built to generate four prostate urine risk (PUR) signatures for predicting the probability of normal tissue (PUR‐1), D'Amico low‐risk (PUR‐2), intermediate‐risk (PUR‐3), and high‐risk (PUR‐4) prostate cancer. This model was applied to a test cohort (n = 177) for diagnostic evaluation, and to an AS sub‐cohort (n = 87) for prognostic evaluation. Results Each PUR signature was significantly associated with its corresponding clinical category (P ˂ 0.001). PUR‐4 status predicted the presence of clinically significant intermediate‐ or high‐risk disease (area under the curve = 0.77, 95% confidence interval [CI] 0.70–0.84). Application of PUR provided a net benefit over current clinical practice. In an AS sub‐cohort (n = 87), groups defined by PUR status and proportion of PUR‐4 had a significant association with time to progression (interquartile range hazard ratio [HR] 2.86, 95% CI 1.83–4.47; P ˂ 0.001). PUR‐4, when used continuously, dichotomized patient groups with differential progression rates of 10% and 60% 5 years after urine collection (HR 8.23, 95% CI 3.26–20.81; P ˂ 0.001). Conclusion Urine‐derived EV‐RNA can provide diagnostic information on aggressive prostate cancer prior to biopsy, and prognostic information for men on AS. PUR represents a new and versatile biomarker that could result in substantial alterations to current treatment of patients with prostate cancer.
Oncolytic viruses are replication competent, tumor selective and lyse cancer cells. Their potential for anti-cancer therapy is based upon the concept that selective intratumoral replication will produce a potent anti-tumor effect and possibly bystander or remote cell killing, whilst minimizing normal tissue toxicity. Viruses may be naturally oncolytic or be engineered for oncolytic activity, and possess a host of different mechanisms to provide tumor selectivity. Clinical use of live replicating viruses is associated with a unique set of safety issues. Clinical experience has so far provided evidence of limited efficacy and a favourable toxicity profile. The interaction with the host immune system is complex. An anti-viral immune response may limit efficacy by rapidly clearing the virus. However, virally-induced cell lysis releases tumor associated antigens in a 'dangerous' context, and limited evidence suggests that this can lead to the generation of a specific anti-tumor immune response. Combination therapy with chemotherapy or radiotherapy represents a promising avenue for ongoing translation of oncolytic viruses into clinical practice. Obstacles to therapy include highly effective non-specific host mechanisms to clear virus following systemic delivery, immune-mediated clearance, and intratumoral barriers limiting virus spread. A number of novel strategies are now under investigation to overcome these barriers. This review provides an overview of the potential role of oncolytic viruses, highlighting recent progress towards developing effective therapy and asks if they are a realistic therapeutic option at this stage.
Chromosome 8q24 is a susceptibility locus for multiple cancers, including prostate cancer. Here we combine genetic data across the 8q24 susceptibility region from 71,535 prostate cancer cases and 52,935 controls of European ancestry to define the overall contribution of germline variation at 8q24 to prostate cancer risk. We identify 12 independent risk signals for prostate cancer (p
Background: Adjuvant sunitinib significantly improved disease-free survival (DFS) versus placebo in patients with locoregional renal cell carcinoma (RCC) at high risk of recurrence after nephrectomy (hazard ratio [HR] 0.76, 95% confidence interval [CI] 0.59–0.98; p = 0.03). Objective: To report the relationship between baseline factors and DFS, pattern of recurrence, and updated overall survival (OS). Design, setting, and participants: Data for 615 patients randomized to sunitinib (n = 309) or placebo (n = 306) in the S-TRAC trial. Outcome measurements and statistical analysis: Subgroup DFS analyses by baseline risk factors were conducted using a Cox proportional hazards model. Baseline risk factors included: modified University of California Los Angeles integrated staging system criteria, age, gender, Eastern Cooperative Oncology Group performance status (ECOG PS), weight, neutrophil-to-lymphocyte ratio (NLR), and Fuhrman grade. Results and limitations: Of 615 patients, 97 and 122 in the sunitinib and placebo arms developed metastatic disease, with the most common sites of distant recurrence being lung (40 and 49), lymph node (21 and 26), and liver (11 and 14), respectively. A benefit of adjuvant sunitinib over placebo was observed across subgroups, including: higher risk (T3, no or undetermined nodal involvement, Fuhrman grade 2, ECOG PS 1, T4 and/or nodal involvement; hazard ratio [HR] 0.74, 95% confidence interval [CI] 0.55–0.99; p = 0.04), NLR 3 (HR 0.72, 95% CI 0.54–0.95; p = 0.02), and Fuhrman grade 3/4 (HR 0.73, 95% CI 0.55– 0.98; p = 0.04). All subgroup analyses were exploratory, and no adjustments for multiplicity were made. Median OS was not reached in either arm (HR 0.92, 95% CI 0.66–1.28; p = 0.6); 67 and 74 patients died in the sunitinib and placebo arms, respectively. Conclusions: A benefit of adjuvant sunitinib over placebo was observed across subgroups. The results are consistent with the primary analysis, which showed a benefit for adjuvant sunitinib in patients at high risk of recurrent RCC after nephrectomy. Patient summary: Most subgroups of patients at high risk of recurrent renal cell carcinoma after nephrectomy experienced a clinical benefit with adjuvant sunitinib. Trial registration: ClinicalTrials.gov NCT00375674.
Reovirus type 3 Dearing (Reolysin, Oncolytics Biotech) is a wild-type double-stranded RNA virus that is ubiquitous and nonpathogenic in humans. It has been shown to be oncolytic by its ability to replicate in transformed cells but not in normal cells. Reovirus has been shown to exert significant antitumor effects in both preclinical in vitro and in vivo studies. In addition, reovirus can activate both innate and adaptive antitumor response against human and murine tumors. However, despite antitumor activity, the responses to reovirus monotherapy in human trials have been modest and short-lived. As a result, a number of potential strategies for improving antitumor efficacy are currently being evaluated. This chapter describes the application of oncolytic reovirus as an anticancer agent, alone or in combination with conventional therapies such as radiotherapy and chemotherapeutics. It also summarizes current clinical trials on reovirus therapy. © 2014 Elsevier Inc. All rights reserved.
Objectives: Prostate-specific-antigen (PSA) screening resulted in reduced prostate cancer (PCa) mortality in a large clinical trial, but due to many false positives and overdiagnosis of indolent disease, many guidelines do not endorse universal screening and instead recommend an individualized decision based on each patient’s risk. We sought to develop and validate a genetic tool to predict age of aggressive PCa onset and to guide decisions of whom to screen and at what age. Design: Genotype, PCa status, and age were analyzed to select single-nucleotide polymorphisms (SNPs) associated with PCa diagnosis. These SNPs were incorporated into a survival analysis to estimate their effects on age at diagnosis of aggressive PCa (i.e., not eligible for surveillance per NCCN Guidelines; any of: Gleason score ≥7, stage T3-T4, PSA ≥10, nodal metastasis, distant metastasis). The resulting polygenic hazard score (PHS) is an assessment of individual genetic risk. The final model was applied to an independent dataset containing genotype and screening PSA data. PHS was calculated for these men to test prediction of PCa-free survival. Setting: Multiple, international PRACTICAL consortium member institutions. Participants: All PRACTICAL consortium participants of European ancestry with known age, PCa status, and quality-assured iCOGS array genotype data. Development dataset comprised 31,747 men. Validation dataset comprised 6,411 men. Main outcome measures: PHS prediction of age of onset of aggressive PCa in validation set. Results: In the independent validation set, PHS calculated from 54 SNPs was a highly significant predictor of age at diagnosis of aggressive PCa (z=11.2, p98th percentile) were compared to those with average PHS (30th-70th percentile), the hazard ratio for aggressive PCa was 2.9. Conclusions:Polygenic hazard scores give personalized genetic risk estimates that predict for age of onset of aggressive PCa.